Metastatic Nasopharyngeal Carcinoma
Definition
Carcinoma of the nasopharynx metastatic to lymph nodes.
Synonym
Lymphoepithelioma.
Epidemiology
Nasopharyngeal carcinoma (NPC) is endemic in southern China (including Hong Kong), Malaysia, northern Africa, and in Alaskan Eskimos (1,2). In southern China, the incidence of NPC has been reported to be approximately 25 per 100,000 males, representing 15–20% of all malignant neoplasms (3). In the United States and western Europe, NPC occurs sporadically and the incidence is low, representing approximately 0.25% of all malignant neoplasms and 5% of all head and neck carcinomas (1,2,3).
Pathogenesis
The pathogenesis of NPC is related to environmental and genetic factors and Epstein-Barr virus (EBV) infection. The existence of geographic regions endemic for NPC argues for environmental factors that may be involved in pathogenesis (1,2,3). These factors overlap with or augment the role of EBV infection. In addition, individuals from endemic regions who relocate to nonendemic regions retain an increased risk of developing NPC, suggesting a genetic component to pathogenesis.
In regions where NPC is endemic, EBV infection occurs early in life and may remain latent for 40 to 60 years before tumors arise (4). Sera from patients with NPC have elevated titers of immunoglobulin (IgG) antibody against early EBV antigen and IgA antibodies against EBV viral capsid antigen (1,2,4). These antibodies can be detected before onset of NPC and correlate with a high risk for developing NPC.
Evidence of EBV infection in NPC can be shown using immunohistochemical, in situ hybridization, or molecular techniques. The latter have shown that EBV is monoclonal, suggesting that infection occurs prior to clonal expansion and, therefore, early in pathogenesis (5). One hypothesis is that EBV is required for the initiation of carcinogenesis, but that other genetic events are also necessary for the fully malignant phenotype (6). Epstein-Barr virus infection is constant in all histologic types of NPC, and in both primary and metastatic neoplasms, in endemic regions. In non-endemic regions, EBV can be absent, particularly in keratinizing tumors.
Clinical Syndrome
Patients with NPC in the United States have a bimodal age-incidence curve, with peaks between 15 and 25 years of age, and between 60 and 69 years of age. (7). Males are affected more frequently than females, with a ratio of over 2-to-1 in younger patients (8). Depending on the exact location within the nasopharynx, symptoms and signs vary. In a retrospective analysis of almost 5,000 patients, the most common symptoms were neck mass (76%), nasal dysfunction (73%), ear dysfunction (62%), headache (35%), diplopia (11%), facial numbness (8%), and weight loss (7%) (1). The most common physical signs were one or more enlarged cervical lymph nodes (76%) and cranial nerve palsies (20%). The cranial nerves commonly involved were the third, fifth, sixth, and twelfth (1).
Primary NPC can be very small and difficult to identify by endoscopy. Even if not seen grossly, blind biopsy is recommended in suspected patients. Primary tumors may only be identified after repeated examinations. In some patients, NPC has not been detected until autopsy and even then the lesions were inconspicuous and appeared only as slightly raised, ill-defined granular patches of the nasopharyngeal or oropharyngeal mucosa. Nasopharyngeal carcinoma most commonly arises in the roof and lateral walls of the nasopharynx, and less often in the posterior wall (2,9). The fossa of Rosenmüller, a recess posterior to the opening of the eustachian tubes, can be difficult to examine by endoscopy and is an infamous site of origin. The inaccessibility of the primary site contributes to the late diagnosis of NPC, after the disease has spread.
Nasopharyngeal carcinoma is notorious for metastases to cervical lymph nodes, usually superior deep cervical lymph nodes, and detection of nodal metastases is commonly the first sign of NPC (10). Cervical lymph node metastases are most often unilateral, but can be bilateral in one-third of cases (2,11). The frequent bilaterality is explained by the central location of the primary tumor. In tumor-node-metastasis (TNM) staging of NPC, lymph nodes are classified into four groups: N0, no evidence of lymph node metastases; N1, unilateral nodal metastases, less than 6 cm, above the supraclavicular fossa; N2, bilateral nodal metastases, less than 6 cm, above the supraclavicular fossa; N3, metastases greater than 6 cm (A) or extending into the supraclavicular fossa (B) (2).
The advent of improved imaging studies has greatly improved the identification of primary NPC, as well as the staging of these patients. Computed tomography and magnetic resonance imaging studies can now define with far greater precision (relative to standard radiographs and endoscopy) the sites of involvement and patterns of spread. Improved localization has facilitated more directed radiotherapy and the improved stratification of patients for radiotherapy and/or chemotherapy regimens (2).
Tumors that closely resemble NPC can arise in the palatine and lingual tonsils, thymus, and larynx, an observation that has led some authors to suggest the name undifferentiated carcinoma of nasopharyngeal type for the whole group (12). The suggested protocol for the management of patients with cervical lymphadenopathy without an obvious primary site of origin starts with fine needle aspiration to establish a cytologic diagnosis. In cases of squamous cell carcinoma in an upper cervical lymph node, panendoscopy is indicated, including biopsy of all suspected areas and blind biopsies of the common primary
sites—nasopharynx, tonsil, base of the tongue, supraglottic larynx, and piriform sinus (13).
sites—nasopharynx, tonsil, base of the tongue, supraglottic larynx, and piriform sinus (13).
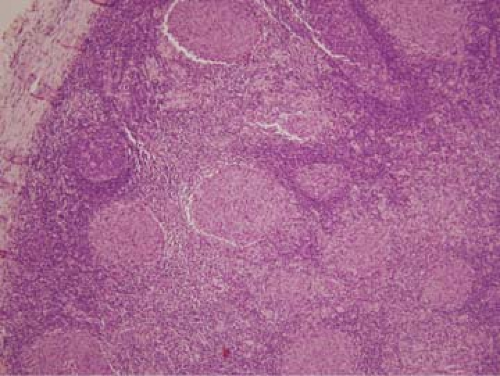 Figure 89.1. Metastatic nasopharyngeal carcinoma, nonkeratinizing differentiated type in cervical lymph node. Islands of neoplasm are interspersed with lymphoid tissue in this field. Hematoxylin-eosin stain, × 100.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|