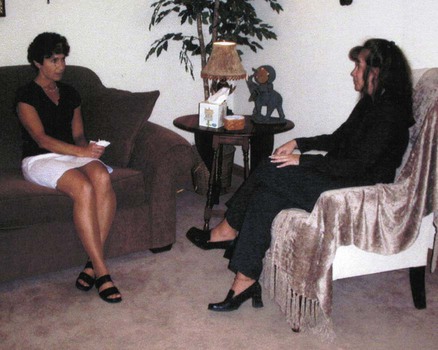
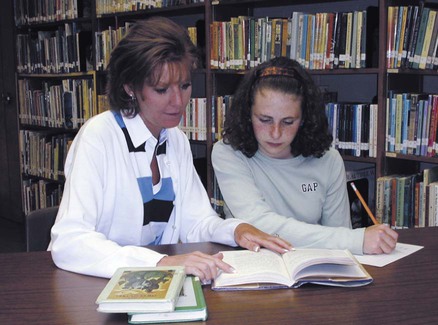
After studying Chapter 14, you should be able to: 1. Name some contributing factors to mental disorders. 2. List some of the many causes of mental retardation. 3. Describe the characteristic manifestations of pervasive development disorders including autism. 4. List criteria for diagnosis of attention-deficit hyperactivity disorder. 5. List some examples of tic disorders. 6. Describe the progressive degenerative changes in an individual with Alzheimer’s disease. 7. Explain important factors in the treatment of Alzheimer’s disease. 8. Explain the cause of vascular dementia. 9. Relate treatment options for alcohol abuse. 10. Name the classic signs and symptoms of schizophrenia. Explain what is included in the multidimensional treatment plan. 11. Explain why bipolar disorder is considered a major affective disorder. Describe the treatment approach. 12. Explain the difference between reactive depression and major depressive disorder. 13. Name the distinguishing characteristics of personality disorders. 14. Discuss how each type of anxiety disorder prevents a person from leading a normal life. 15. Explain how posttraumatic stress disorder differs from other anxiety disorders. 16. Explain how a somatization disorder is diagnosed. 17. Discuss the relationship between anxiety and conversion disorder. 18. Describe Münchausen’s syndrome. 19. Contrast insomnia to narcolepsy. Psychological pain is real and intense and can affect physical health. Subsequently, impaired or pathologic coping skills emerge in people’s behavior. Some coping behaviors are conscious, and some are not easily controlled because they are unconscious. Certain disorders in thinking, perceiving, and behaving can be organized into clusters of signs and symptoms. These clusters become diagnostic criteria and a part of a total physical and psychological evaluation. The American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders, fourth edition (DSM-IV) (Figure 14-1) E14-2, is the accepted reference that offers guidelines for criteria to be used in the clinical setting when diagnosing a mental disorder. In addition to diagnostic criteria, the DSM-IV gives the practitioner a standardized diagnostic code, similar to the International Classification of Diseases, ninth revision, Clinical Modification (ICD-9-CM and ICD-10-CM) coding systems. E14-3 Modern therapeutic approaches include control of symptoms with psychotropic drugs, including antipsychotic drugs, antidepressants, anxiolytics (antianxiety agents), central nervous system (CNS) stimulants, and antimanic agents; hospitalization during acute episodes; psychotherapy; electroconvulsive therapy; and group therapy. Outpatient treatment is available and preferred in many cases (Figure 14-2). Play therapy is included in counseling sessions for some children. (See the Enrichment box on play therapy.) Patients with mental illnesses and conditions need established routines and consistency in treatment and daily living activities. Axis I: Mood and thought disorders, which often respond to medication and psychotherapy. Axis II: Mental retardation and personality disorders. Many third-party providers currently do not reimburse for Axis-II disorders. Axis III: Medical conditions that contribute to the psychological condition. Axis IV: Stressors that contribute to the psychological condition. Axis V: GAF (Global Assessment of Functioning). This is a number, 0 to 100, that indicates level of functioning with 0 representing the lowest level of functioning and 100 representing the highest. Some children who are learning disabled also may be diagnosed with hyperactivity and therefore may respond to drug therapy, usually with stimulants. Other children may respond favorably to special instructional techniques (Figures 14-3 and 14-4). Continuing research is attempting to help develop additional treatments for children with learning disabilities. E14-6 The three subtypes are listed as follows: Attention-Deficit/Hyperactivity Disorder Predominantly Inattentive Type: This subtype is used if six (or more) symptoms of inattention (but fewer than six symptoms of hyperactivity-impulsivity) have persisted for at least 6 months. Attention-Deficit/Hyperactivity Disorder Predominantly Hyperactive-Impulsive Type: This subtype should be used if six (or more) symptoms of hyperactivity-impulsivity (but fewer than six of inattention) have persisted for at least 6 months. Attention-Deficit/Hyperactivity Disorder Combined Type: This subtype should be used if six (or more) symptoms of inattention and six (or more) symptoms of hyperactivity-impulsivity have persisted for at least 6 months.
Mental Disorders
Mental Wellness and Mental Illness
Learning Disorders
Treatment
Attention-Deficit Hyperactivity Disorder
Symptoms and Signs
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree