Prostate-Specific Antigen Velocity
- PSA velocity (PSAV), the rate of change in PSA over time, is abnormal when it is >0.35 ng/mL/year (for tPSA <4 ng/mL) or >0.75 ng/mL/year (for tPSA >4).
- It correlates with prostate cancer diagnosis and is most reliable when three values are obtained at the same laboratory over at least 18 months. High PSAV, however, may be indicative of prostatitis.
- One study suggests that PSAV may be prognostic when obtained in the year before the diagnosis of prostate cancer.15
Free Prostate-Specific Antigen
- Percent-free PSA (fPSA), the ratio of free circulating to bound PSA in serum, is lower in men with prostate cancer than in those with benign prostatic diseases.
- It is most useful in deciding which patients with a mildly elevated PSA (4 to 10 ng/mL) should undergo biopsy.
- An upper cutoff of 30% significantly decreases the number of false-positive biopsies while maintaining a high level of sensitivity.16
- The complexed PSA (cPSA) is also measurable, but has no significant advantage over fPSA.
Prostate-Specific Antigen Density
- Defined as the PSA divided by prostate volume (measured by transrectal ultrasound or MRI) and compared with age-/race-specific reference ranges
- More costly and has less clear benefit on cancer detection rates. Not currently a part of routine guidelines
Screening
- The decision as to whether to screen for prostate cancer must be individualized, as the lack of evidence from clinical trials has led to very different recommendations on screening. Patients who request screening must be educated about the risks and benefits involved. (Fig. 4-1).
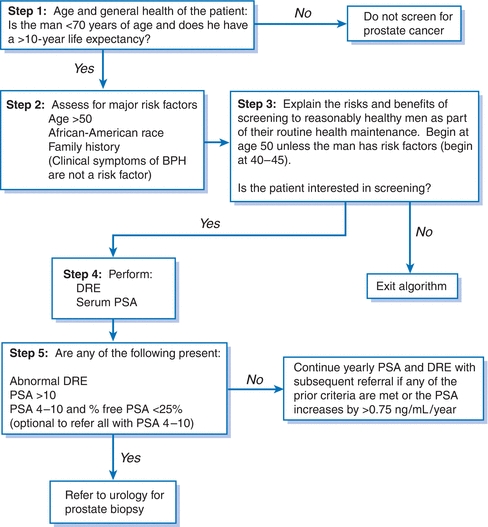
Figure 4-1 Prostate cancer screening algorithm. BPH, benign prostatic hyperplasia; DRE, digital rectal examination; PSA, prostate-specific antigen.
- The USPSTF 2012 update concludes that there is moderate certainty that the benefit of screening does not outweigh potential harm and recommends against PSA-based screening for prostate cancer. Men who request screening should be educated to enable an informed choice.
- The American Cancer Society recommends screening for men at age 50 if life expectancy is at least 10 years. The frequency should be annual if PSA is >2.5 ng/mL and every 2 years if PSA is <2.5 ng/mL. Men at high risk (African American men or men with one or more first-degree relatives with prostate cancer prior to age 65) should be offered screening starting at age 40 to 45.
- The American Urological Association recommends an individualized approach and shared decision making for men 55 to 69 years old.
Benign Prostatic Hyperplasia
GENERAL PRINCIPLES
- Benign prostatic hyperplasia (BPH) is defined histologically as hypertrophy of glandular and stromal tissue.
- It is present primarily in older men with functioning testicles. The prevalence of BPH increases with age from 8% among men in their fourth decade of life to 80% among those >80 years of age, with lower urinary tract symptoms (LUTS) in about 25% to 45% of men >70 years of age.17
- BPH may be complicated by recurrent urinary tract infections (UTIs), urinary bladder stones, and acute urinary retention.
DIAGNOSIS
Clinical Presentation
History
- Patients with LUTS complain of urgency, frequency, nocturia, weak stream, hesitancy, and incomplete emptying.
- The American Urological Association Symptom Index (AUA-SI) (Table 4-2), a standardized questionnaire that quantifies these symptoms, should be administered to all men with BPH.18 The AUA-SI score is used to classify symptom severity, guide treatment recommendations, and follow response to therapy.
- The history should also assess for sexual dysfunction, neurogenic bladder; prior urethral trauma or urethritis; diabetes; hematuria; family history of BPH or prostate cancer; and drugs that decrease bladder function or increase tone at bladder neck (anticholinergics, sympathomimetic amines).
TABLE 4-2 American Urological Association Symptom Index
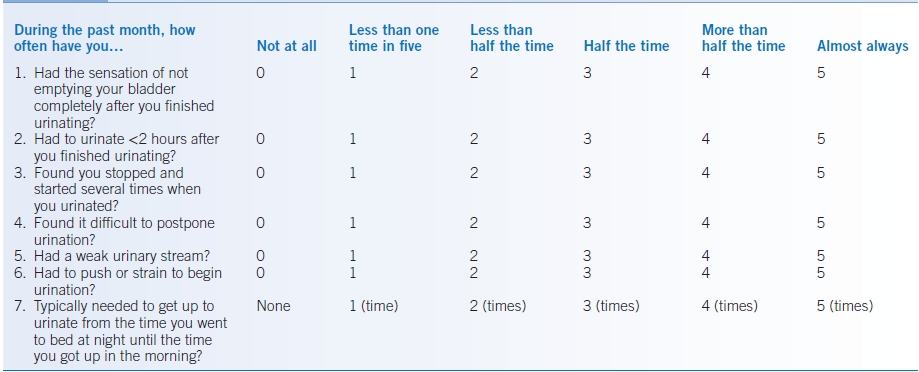
0–7 points = mild symptoms8–19 points = moderate symptoms20–35 points = severe symptomsModified from Barry MJ, Fowler FJ Jr, O’Leary MP, et al. The American Urological Association Symptom Index for benign prostatic hyperplasia. The Measurement Committee of the American Urological Association. J Urol 1992;148:1549.
Physical Examination
The prostate should be palpated for nodules and an estimation of its size. Men with oversized prostates are at increased risk of experiencing complications and undergoing prostate surgery.
Diagnostic Testing
Laboratories
- Urinalysis should be obtained to rule out infection and assess for complications (hematuria, UTI) and glycosuria.
- Serum creatinine should be obtained as it may indicate underlying kidney disease, which could contribute to LUTS.
- Screening for prostate cancer is optional, as its prevalence is not increased despite the fact that PSA is elevated in 25% to 30% of men with BPH.
- PSA is predictive of prostate size, as PSA values of >1.6, 2.0, and 2.3 correlate with 70% sensitivity and specificity to prostates >40 mL in size in men in their 50s, 60s, and 70s, respectively.19
Imaging
Renal imaging (ultrasound or intravenous pyelography) should be performed in patients with complications such as hematuria, recurrent UTIs, or unexplained chronic kidney disease.
Diagnostic Procedures
Urodynamic testing (peak flow rate and pressure volume studies) should be reserved for patients with an unclear diagnosis, suspected neurogenic bladder dysfunction, or moderate to severe disease that fails to respond to initial therapy.
TREATMENT
- The major factors to consider in selecting a therapy are AUA-SI score and prostate size. The other factors to consider are age, concomitant hypertension, current medications, sexual history, and the degree to which the symptoms affect quality of life.
- Watchful waiting without treatment is recommended for patients with mild symptoms (AUA-SI ≤7) and is an option for those with moderate symptoms who do not want to initiate lifelong medical therapy and do not have BPH complications (urinary retention, renal insufficiency, or UTI).
- Patients should minimize fluids before bedtime and avoid medications with anticholinergic or sympathomimetic properties (including antihistamines, tricyclic antidepressants, and decongestants), caffeinated beverages, and alcohol.
- Many patients with mild symptoms have no change or improve without treatment; however, there is some concern that delay in treatment may result in bladder decompensation.20
Medications
Pharmacologic therapy is recommended for patients with moderate symptoms who request treatment and for those with severe symptoms.
First-Generation α-Blockers
- Terazosin and doxazosin are α1-adrenergic blockers that relax smooth muscle cells in the prostate and lead to an improvement of symptoms (decrease of 4 to 6 points on AUA-SI) within weeks of initiating therapy.21
- Symptomatic improvement is maintained with long-term therapy, but α1-blockers do not decrease prostate size, the rate of urinary retention, the need for surgery, or PSA.
- α1-Blockers are effective in men with small and large prostates.
- These agents are possible choices for men with concomitant hypertension that requires treatment. Terazosin and doxazosin decrease blood pressure (BP) by approximately 10 to 15/10 to 15 mm Hg in men with elevated BP but have no clinically significant effect on BP in normotensive patients.22 However, they should not be used at the expense of other drugs for overriding indications (see Chapter 6).
- Treatment is initiated at night with dose titration over 2 to 3 weeks to minimize side effects.
- Terazosin is titrated weekly from 1 to 2 to 5 mg PO nightly and can subsequently be increased to 10 to 20 mg PO nightly.
- Doxazosin is titrated from 1 to 2 to 4 mg PO nightly and can be subsequently increased to 8 to 16 mg PO nightly.
- Terazosin is titrated weekly from 1 to 2 to 5 mg PO nightly and can subsequently be increased to 10 to 20 mg PO nightly.
- Common side effects are dizziness, orthostatic hypotension, and fatigue. Hypotension and orthostasis are exacerbated with concomitant use of phosphodiesterase inhibitors for ED (e.g., sildenafil, vardenafil, tadalafil).
- The Food and Drug Administration (FDA) has posted a drug safety alert indicating that α1-blockers increase the risk of floppy iris syndrome in patients with cataract surgery.
Second-Generation α-Blockers
- Alfuzosin, silodosin, and tamsulosin are uroselective α1a-blockers with pharmacologic activity that is limited to the prostate with minimal systemic effects on BP. They are good choices for men who want rapid symptom relief and who are prone to orthostasis.
- The dose for alfuzosin is 10 mg PO daily, silodosin is 8 mg PO daily, and tamsulosin is 0.4 to 0.8 mg PO daily.
- Dose titration and nocturnal dosing are unnecessary for these three agents.
- The dose of silodosin should be halved for patients with a creatinine clearance of 30 to 49 mL/minute.
- Both silodosin and alfuzosin should be avoided in patients with a creatinine clearance of <30 mL/minute.
- Dose titration and nocturnal dosing are unnecessary for these three agents.
- Common side effects of these agents are ejaculatory problems and dizziness.
- The FDA has posted a drug safety alert indicating that tamsulosin and other α1-blockers increase the risk of floppy iris syndrome in patients with cataract surgery.
5α-Reductase Inhibitors
- Finasteride and dutasteride are 5α-reductase inhibitors that inhibit conversion of testosterone to dihydrotestosterone (DHT), reverse epithelial glandular hyperplasia, and shrink the prostate by approximately 15% to 30% within several months.
- Symptomatic improvement is sustained long term, and they are the only drug class that have been shown to decrease the rate of urinary retention and need for prostate surgery.23–25
- These agents are more effective in men with prostates >40 mL in size.26
- PSA can predict which patients are candidates for treatment with finasteride (see the Prostate-Specific Antigen section).
- The symptomatic response to these agents is delayed for 6 to 12 months.
- The dose for finasteride is 5 mg PO daily, and for dutasteride, it is 0.5 mg PO daily.
- The only common side effects are sexual, including ED, decreased libido, and ejaculatory dysfunction.
- After 6 months of therapy, finasteride decreases PSA by approximately 50%.
- PSA may still be used as a screening test for prostate cancer provided that the PSA value is doubled.27
- Free PSA is unchanged by treatment.
- PSA may still be used as a screening test for prostate cancer provided that the PSA value is doubled.27
- Questions have been raised about the safety of these agents in the Prostate Cancer Prevention Trial. This 7-year study showed that, compared with placebo, finasteride reduced the risk of prostate cancer. However, participants who developed prostate cancer while on study drug were more likely to develop higher-grade cancers.28,29 The FDA recommends that patients be assessed for prostate cancer before starting this class of drugs.
Combination Therapy
- Combination therapy with an α1-blocker and finasteride makes theoretical sense for men with large prostates and is frequently attempted, but research study results are mixed.
- It is a general practice among many to use combination therapy in symptomatic men with large prostate and monotherapy (α1-blockers) in patients with small gland size.30,31
Herbal Treatment
- Several different forms of herbal therapy, including saw palmetto (Serenoa repens), Pygeum africanum, Cernilton, and β-sitosterols, are available and self-prescribed by patients to treat BPH.
- These agents have been shown to be effective in the short term, but their mechanism of action and long-term efficacy are unknown.32
- Saw palmetto (160 mg PO bid) is the most commonly used herb in the United States, but is not FDA approved.
Surgical Management
- Indications for referral to urology include refractory LUTS, complications such as recurrent hematuria or recurrent UTIs, bladder stones, acute urinary retention and renal insufficiency with hydronephrosis, a rectal examination or PSA suspicious for prostate cancer, and an unclear diagnosis when urodynamic testing may be helpful.
- Transurethral resection of the prostate (TURP), the “gold standard” for BPH treatment, has a much greater benefit in reducing symptoms than medical therapy.
- TURP results in retrograde ejaculation and ED in a significant percentage of patients, and approximately 20% have unsatisfactory results and require further therapy.
- As TURP removes only central prostatic tissue, it does not eliminate the chance of developing prostate cancer.
- Several new minimally invasive surgical procedures have been introduced as alternatives to TURP.
- TURP results in retrograde ejaculation and ED in a significant percentage of patients, and approximately 20% have unsatisfactory results and require further therapy.
Prostatitis
GENERAL PRINCIPLES
- Prostatitis is the most common urologic complaint among men <50 years of age.
- The prostatitis syndromes are classified by the acuity of presentation and findings on urinalysis and culture before and after prostatic massage.
- Prostatitis is classified as follows:
- Acute prostatitis
- Chronic bacterial prostatitis
- Chronic prostatitis/chronic pelvic pain syndrome:
- Inflammatory
- Noninflammatory
- Inflammatory
- Acute prostatitis
- Asymptomatic inflammation of the prostate
- Only 5% to 10% of cases are due to bacterial causes.33
DIAGNOSIS
Acute Bacterial Prostatitis
- Patients present with symptoms of a UTI (e.g., dysuria, frequency, urgency) and systemic symptoms such as fever, malaise, and lower abdominal or back pain. Risk factors include instrumentation and HIV.
- A gentle prostate examination might reveal an enlarged, warm, and very tender prostate. Vigorous massage is contraindicated as this could cause bacteremia and sepsis.
- Urinalysis and culture are positive, most often for Escherichia coli or other gram-negative organisms.
- An abdominal ultrasound or CT scan to rule out a prostatic abscess should be considered if initial treatment fails.
Chronic Prostatitis Syndromes
- Patients with the three chronic prostatitis syndromes present with similar symptoms, classically a triad of recurrent voiding symptoms, pain (pelvic, perineal, inguinal, back, penile, or scrotal), and ejaculatory symptoms (pain, hematospermia).
- Patients with chronic bacterial prostatitis are usually older, frequently have recurrent UTIs with the same organism, and may have a history of acute prostatitis.
- Patients with the two chronic nonbacterial prostatitis syndromes are often younger and do not have a history of recurrent UTIs.
- The predominant symptom of pain and predilection to occur in younger men distinguish it from BPH.
- Chronic nonbacterial prostatitis is the most common urologic diagnosis in men <50 years of age.
- The predominant symptom of pain and predilection to occur in younger men distinguish it from BPH.
- The prostate examination is often normal in men with each of the chronic prostatitis syndromes. A diagnostic prostate massage comparing a midstream urine specimen (the second 10 mL of urine voided) with one after a vigorous prostate massage is the test of choice to correctly diagnose the three syndromes (Table 4-3). However, this is usually done after presumptive diagnosis fails to respond to treatment.
TABLE 4-3 Diagnostic Prostate Massage Results
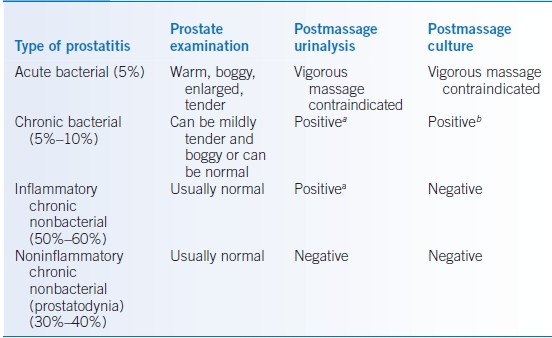
aA positive urinalysis is >10 to 15 WBCs/high-power field.
bA positive culture has a colony count that is at least 10-fold greater than the premassage culture.
TREATMENT
Acute Bacterial Prostatitis
- Patients should be treated initially with broad-spectrum parenteral antibiotics followed by oral agents if they respond.
- Potential oral regimens include trimethoprim-sulfamethoxazole, 1 DS tablet PO bid; doxycycline, 100 mg PO bid; ciprofloxacin, 500 mg PO bid; or levofloxacin, 500 mg PO daily for 4 to 6 weeks.
- Severely ill patients with suspected bacteremia require admission for IV antibiotics.
- Potential oral regimens include trimethoprim-sulfamethoxazole, 1 DS tablet PO bid; doxycycline, 100 mg PO bid; ciprofloxacin, 500 mg PO bid; or levofloxacin, 500 mg PO daily for 4 to 6 weeks.
- Supportive care with analgesics, stool softeners, and vigorous oral hydration may be beneficial.
- Because of the relatively high risk for urinary retention, bladder scanning should be done to assess the postvoid residual. For patients who require short-term drainage, a small urethral catheter may be sufficient; those who require long-term drainage will need a suprapubic catheter.
Chronic Bacterial Prostatitis
- Prolonged courses of antibiotics (4 to 6 weeks), preferably with a fluoroquinolone (excellent prostate penetration), are recommended.
- α1-Adrenergic blockers (see the “Benign Prostatic Hyperplasia” section above) may provide additional symptomatic relief.
- Recurrences require retreatment.
Chronic Nonbacterial Prostatitis
- Treatment of both types of chronic nonbacterial prostatitis is difficult and often prolonged. Recommendations are based primarily on clinical experience, as controlled trial data are limited.34
- Patients with inflammatory chronic nonbacterial prostatitis should receive a trial of 4 to 6 weeks of antibiotics (fluoroquinolone or trimethoprim-sulfamethoxazole). This should be continued for 12 weeks if improvement occurs due to anecdotal evidence that links the syndrome to atypical pathogens. Doxycycline and azithromycin can be used to treat Chlamydia trachomatis.
- Treatment options for noninflammatory chronic nonbacterial prostatitis (prostatodynia) include α1-adrenergic blockers, nonsteroidal anti-inflammatory drugs, “muscle relaxants” such as diazepam, and anticholinergic agents.35
Erectile Dysfunction
GENERAL PRINCIPLES
- ED is the consistent inability to attain or maintain an erection that is satisfactory for successful intercourse.36
- The prevalence increases with advancing age, and the impact on quality of life is substantial.37
- Many men are embarrassed to raise the subject, so it is important that primary care physicians initiate the conversation with their patients.
- The risk factors for ED are presented in Table 4-4.
TABLE 4-4 Common Risk Factors for Erectile Dysfunction
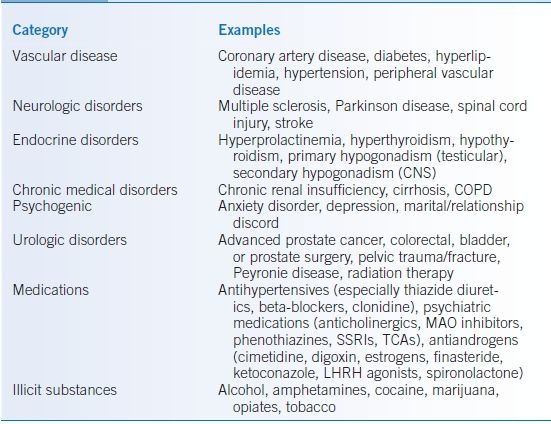
CNS, central nervous system; COPD, chronic obstructive pulmonary disease; LHRH, luteinizing hormone–releasing hormone; MAO, monoamine oxidase; SSRIs, selective serotonin reuptake inhibitors; TCAs, tricyclic antidepressants.
DIAGNOSIS
Clinical Presentation
History
- A detailed sexual history should assess the severity, onset, duration, progression, and situational nature of the problem to confirm that the patient has erectile failure and not a problem with libido or ejaculation.
- A gradual progressive onset of ED with absence of nocturnal or morning erections suggests an underlying medical cause.
- ED that develops suddenly is likely either psychogenic or due to a medication.
- Risk factors for ED should be reviewed (Table 4-4).
- The potential cardiovascular risk of intercourse to the patient should be assessed, given the strong association between ED and coronary artery disease. Sexual activity is equivalent to walking 1 mile in 20 minutes, climbing two flights of stairs in 10 seconds, or 3 metabolic equivalents (METs) of activity.38
- Patients who can safely exercise to a level of five METs (see Chapter 2, Table 2-3) are at low risk for coronary ischemia during intercourse. Stress testing should be considered, before the initiation of therapy or resumption of intercourse, in sedentary men with multiple cardiac risk factors who cannot safely exercise to this level. Patients should complete 4 minutes on the Bruce treadmill protocol (5 to 6 METs) without symptoms, arrhythmias, or fall in blood pressure.38
Physical Examination
The physical examination should assess for evidence of vascular or neurologic disease, stigmata of hypogonadism (small testicles, gynecomastia), prostate abnormality (with DRE), and penile anatomic abnormalities (Peyronie disease).
Diagnostic Testing
- Routine laboratory evaluation should include serum glucose, renal function, complete blood count, and lipid analysis.
- A PSA should be considered if testosterone therapy needs to be initiated.
- Thyroid-stimulating hormone and liver function tests should be performed if the initial history or physical examination is suggestive of thyroid or liver disease.
- Routine testosterone assessment in patients with ED is controversial.
- Hypogonadism is the cause of ED in 5% to 10% of patients, but only approximately one-third of these patients improve with testosterone replacement.39
- Testing with morning total and free serum testosterone is initially recommended only for patients with low libido or evidence of hypogonadism.
- Testing should otherwise be deferred until patients have failed oral pharmacologic therapy.
- Abnormal initial testosterone levels should be repeated for confirmation along with serum luteinizing hormone (LH), follicle-stimulating hormone (FSH), and prolactin to determine the source of hypogonadism.
- Hypogonadism is the cause of ED in 5% to 10% of patients, but only approximately one-third of these patients improve with testosterone replacement.39
- Urologic testing with nocturnal penile tumescence or vascular studies is unnecessary in the primary care setting.
TREATMENT
- In 80% to 90% of men, erectile function should be restored with some form of therapy.
- Attempts should be made to improve uncontrolled risk factors, such as diabetes and hypertension, and to decrease the use of tobacco, alcohol, and other illicit substances.
- If possible, potentially contributing medications should be stopped or have their doses decreased.
- Reassurance may be curative in young men with psychogenic ED. Referral to a psychologist for marital or couples counseling may be helpful as an adjunctive form of therapy for psychogenic ED that has failed to respond to oral pharmacologic therapy.
Medications
Phosphodiesterase Inhibitors
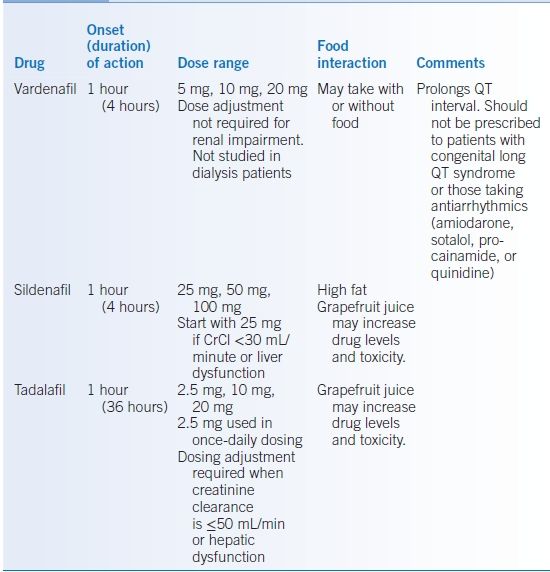
- Phosphodiesterase inhibitors include sildenafil, tadalafil, and vardenafil (Table 4-5).
- These agents are the treatment of choice for ED and work by selectively inhibiting PDE5, which is found in high concentrations within the corpus cavernosum.
- They require sexual stimulation to precipitate an erection and are effective in all forms of organic and psychogenic ED, but response rates are lower in patients with complete ED and diabetes and after radical prostatectomy.40
- They do not increase libido.
- The three agents available are thought to have similar efficacy (no head-to-head trials yet done).
- Side effects include headaches, flushing, dyspepsia, visual disturbance, rhinitis, priapism, and dizziness.
- Patients with symptoms of cardiac disease should be referred for cardiac evaluation before initiation of these agents.
- The PDE5 inhibitors potentiate the effect of nitrates causing severe and refractory hypotension, so the combination of these agents with nitrates in any form (oral, transdermal, IV) is absolutely contraindicated.41
- The combination with α1-adrenergic blockers can also cause orthostatic hypotension and even severe hypotension. Alcohol potentiates the hypotensive effects of these agents.
- They are metabolized in the liver by cytochrome P450 CYP3A4, and thus, caution must be exercised when prescribing with inhibitors such as ketoconazole, itraconazole, protease inhibitors, and cimetidine.
TABLE 4-5 Phosphodiesterase Inhibitors for Erectile Dysfunction
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


