, Arthur H. Cohen2, Robert B. Colvin3, J. Charles Jennette4 and Charles E. Alpers5
(1)
Department of Pathology, Microbiology and Immunology, Vanderbilt University Medical Center, Nashville, Tennessee, USA
(2)
Department of Pathology and Laboratory Medicine, Cedars-Sinai Medical Center, Los Angeles, California, USA
(3)
Department of Pathology Harvard Medical School, Massachusetts General Hospital, Boston, Massachusetts, USA
(4)
Department of Pathology and Laboratory Medicine, University of North Carolina, Chapel Hill, North Carolina, USA
(5)
Department of Pathology, University of Washington, Seattle, Washington, USA
Abstract
Membranoproliferative glomerulonephritis (MPGN) refers to a pattern of injury characterized by diffuse mesangial expansion due to mesangial and endocapillary proliferation and increased mesangial matrix, and thickened capillary walls, often with a double contour “tram-track” appearance [1, 2]. This pattern may be seen with immune complex deposition, or monoclonal proteins, or other organized deposits (as in fibrillary glomerulonephritis). The immune complexes may be undefined in terms of the inciting antigen (“idiopathic”) or secondary to chronic infections [3]. Of note, glomerular basement membrane double contour appearance may be seen in other nonimmune complex injuries, such as the late phase of thrombotic microangiopathy (TMA) or in complement-mediated glomerulonephritides [3]. Although light microscopy may appear similar in these entities, immunofluorescence findings with staining for immunoglobulin and complement and corresponding deposits by electron microscopy readily allow recognition of the immune complexes in MPGN. In contrast, C3 glomerulopathies show C3 staining only, or dominant C3 without significant immunoglobulin, with deposits by electron microscopy, while chronic TMA shows no specific immunofluorescence findings and absence of deposits by electron microscopy. We and others prefer to use the term membranoproliferative glomerulonephritis only for immune complex glomerulonephritides with this pattern [1].
Introduction/Clinical Setting
Membranoproliferative glomerulonephritis (MPGN) refers to a pattern of injury characterized by diffuse mesangial expansion due to mesangial and endocapillary proliferation and increased mesangial matrix, and thickened capillary walls, often with a double contour “tram-track” appearance [1, 2]. This pattern may be seen with immune complex deposition, or monoclonal proteins, or other organized deposits (as in fibrillary glomerulonephritis). The immune complexes may be undefined in terms of the inciting antigen (“idiopathic”) or secondary to chronic infections [3]. Of note, glomerular basement membrane double contour appearance may be seen in other nonimmune complex injuries, such as the late phase of thrombotic microangiopathy (TMA) or in complement-mediated glomerulonephritides [3]. Although light microscopy may appear similar in these entities, immunofluorescence findings with staining for immunoglobulin and complement and corresponding deposits by electron microscopy readily allow recognition of the immune complexes in MPGN. In contrast, C3 glomerulopathies show C3 staining only, or dominant C3 without significant immunoglobulin, with deposits by electron microscopy, while chronic TMA shows no specific immunofluorescence findings and absence of deposits by electron microscopy. We and others prefer to use the term membranoproliferative glomerulonephritis only for immune complex glomerulonephritides with this pattern [1].
This type of immune complex MPGN has previously been referred to as MPGN type I. MPGN typically presents as combined nephritic/nephrotic syndrome with hypocomplementemia. Patients often have progressive renal disease, with about 50 % renal survival at 10 years. Idiopathic MPGN is more common in children and young adults, whereas MPGN-type lesions are more commonly secondary to chronic infections in adults. The so-called MPGN type III may not represent an entity separate from MPGN type I [4, 5]. C3 nephritic factor may be rarely found in these patients, but clinical distinction of this morphology, with frequent subepithelial deposits, has not been apparent.
C3 glomerulopathies include dense deposit disease (DDD), also previously called MPGN type II. Patients with DDD typically have low serum complements, particularly C3, and nephrotic/nephritic syndrome. The majority develop chronic progressive kidney disease. Due to its similar light microscopic appearance, it previously has been classified with MPGN [6]. It is much more rare than MPGN type I, accounting for 15–35 % of total MPGN cases.
C3 glomerulopathies also include a group of patients with deposits with usual appearance by EM, but only C3, or dominant C3, by immunofluorescence. C3 glomerulopathy can affect patients from 7 to 70 years, with average age at presentation 30 years. Patients have proteinuria and microhematuria, with nephrotic syndrome present in around 15 %. The course is variable, with renal function preserved in about half, while about 15 % progress to end-stage kidney disease.
Pathologic Findings
Light Microscopy
Membranoproliferative glomerulonephritis type I characteristically has subendothelial deposits, resulting in a thickened capillary wall and a double contour of the glomerular basement membrane (GBM) by silver stains, and endocapillary proliferation [1].
This appearance results from the so-called circumferential cellular interposition, whereby infiltrating mononuclear cells or even portions of endothelial cells interpose themselves between the endothelium and the basement membrane, with new inner basement membrane being laid down [7]. A circumferential, or partial, double contour basement membrane results. Of note, in nonimmune complex diseases with this appearance by light microscopy (e.g., transplant glomerulopathy, chronic injury after hemolytic uremic syndrome), electron microscopy shows that the double contour results from widening of the GBM due to increased lucency of the lamina rara interna with new basement membrane formed underneath the endothelium. In MPGN type I, the glomeruli show endocapillary proliferation and increased mesangial cellularity and matrix and lobular simplification (Figs. 3.1, 3.2, and 3.3). The term mesangiocapillary glomerulonephritis has also been used for MPGN. Increased mononuclear cells and occasional neutrophils may be present. The proliferation is typically uniform and diffuse in idiopathic MPGN, contrasting the irregular involvement most commonly seen in proliferative lupus nephritis (Fig. 3.1). In secondary forms of MPGN, the injury may be more irregular. Crescents may occur in both idiopathic and secondary forms. Deposits do not involve extraglomerular sites. Lesions progress with less cellularity and more pronounced matrix accumulation and sclerosis over time [8]. Tubular atrophy, interstitial fibrosis, and vascular sclerosis proportional to glomerular scarring are seen late in the course.
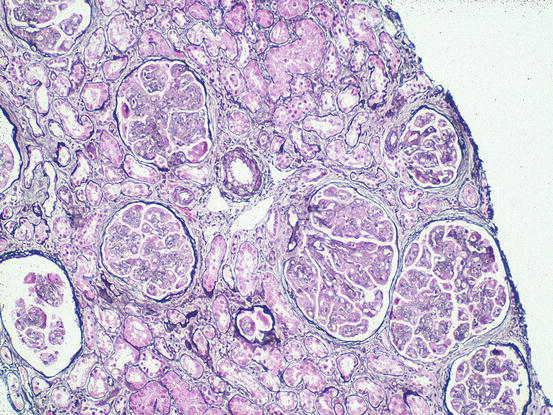
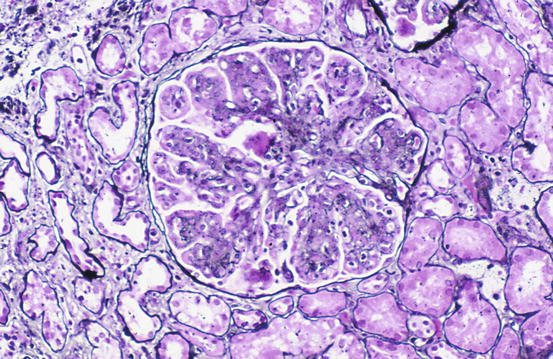
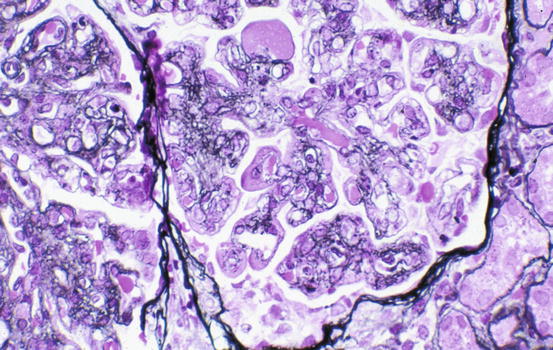
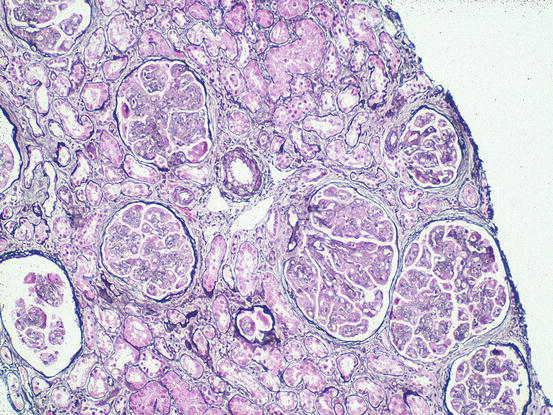
Fig. 3.1
Lobular appearance due to diffuse, global endocapillary proliferation of all glomeruli in immune complex-type membranoproliferative glomerulonephritis (MPGN) (Jones silver stain)
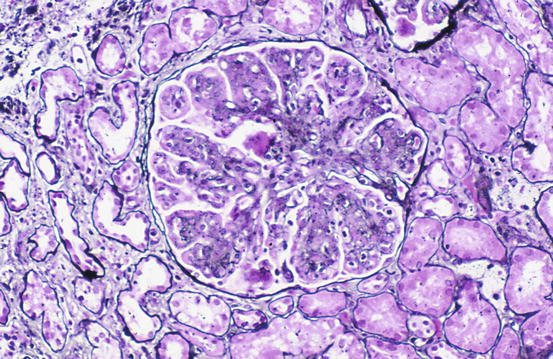
Fig. 3.2
Diffuse, global endocapillary proliferation with extensive glomerular basement membrane (GBM) double contours in immune complex-type MPGN (Jones silver stain)
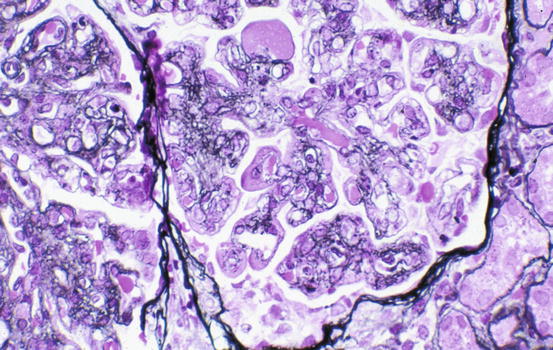
Fig. 3.3
Diffuse, global endocapillary proliferation with GBM double contours and visible large subendothelial deposits in immune complex-type MPGN (Jones silver stain)
Membranoproliferative glomerulonephritis type III shows, in addition to the subendothelial and mesangial deposits, numerous subepithelial deposits.
Diseases with dominant C3 deposits include the C3 glomerulopathies. This group of disorders includes dense deposit disease (DDD, also previously called MPGN type II) and C3 glomerulonephritis [6, 9, 10]. The most common pattern of injury in DDD is mesangial proliferation, followed by endocapillary proliferation (Fig. 3.4) [9]. The basement membranes are thickened and highly refractile and eosinophilic, with involved areas with strings of deposits looking like a string of sausages. The deposits are periodic acid-Schiff (PAS) positive and stain brown with silver stain. Thickening also affects tubular basement membranes and Bowman’s capsule. Crescents may be present. In some cases of C3 glomerulonephritis, the deposits lack the dense appearance by EM of DDD. In these cases, light microscopy most often shows membranoproliferative-type appearance with mesangial and endocapillary proliferation with a nodular appearance in about 20 % of cases.
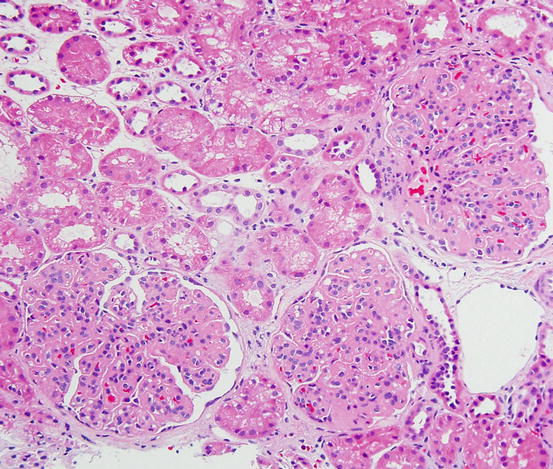
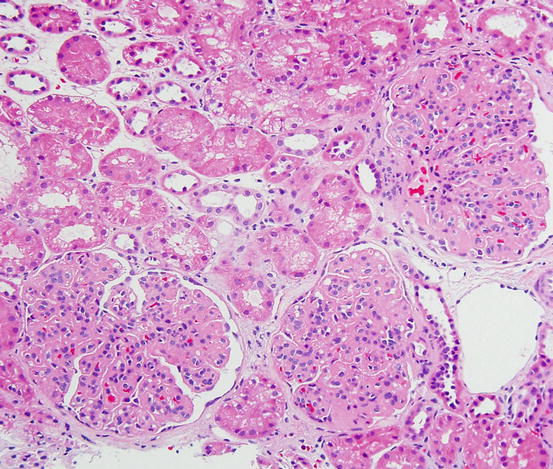
Fig. 3.4
Membranoproliferative pattern in C3 glomerulonephritis (H&E)
Immunofluorescence Microscopy
The immunofluorescence findings are variable in immune complex-type MPGN. Typically, IgG and IgM and C3 are present in an irregular capillary and mesangial distribution (Fig. 3.5). IgA is present in only a small proportion of cases. When C3 staining is dominant, chronic infection or a C3 glomerulopathy should be considered.
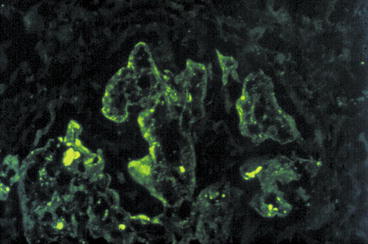
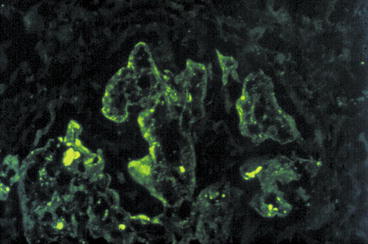
Fig. 3.5
Coarsely granular capillary loop and mesangial deposits in MPGN (anti-IgG antibody immunofluorescence)
In DDD, C3 staining outlines the capillary wall and may be smooth, granular, or discontinuous. Mesangial bright granular staining can be present. Immunoglobulin is usually not detected, indicating the dense deposits are not classic antigen-antibody immune complexes. However, segmental IgM or less often IgG and very rarely IgA have been reported [11].
In non-DDD cases of C3-dominant glomerulonephritis, there are by definition isolated or dominant C3 deposits without significant C1q or immunoglobulin (Fig. 3.6). Deposits mirror the light microscopic pattern, with mesangial and scattered capillary loop deposits.
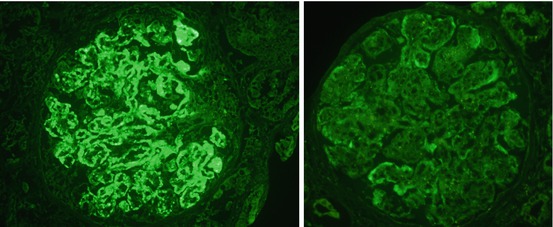
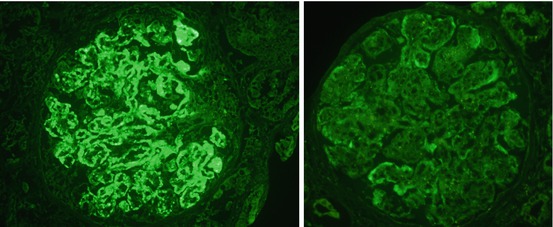
Fig. 3.6
Coarsely granular capillary loop and mesangial deposits in C3 glomerulonephritis, staining dominantly for C3 (left) with negligible staining for IgG (right) (immunofluorescence)
Electron Microscopy
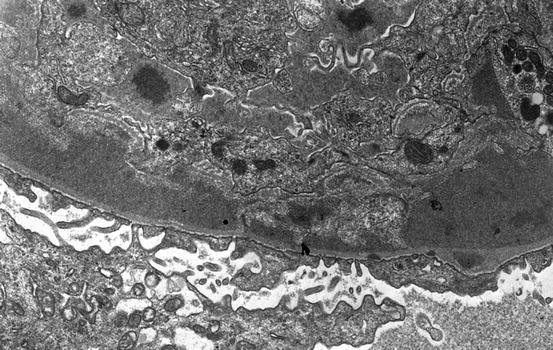
By electron microscopy, immune complex-type MPGN shows numerous dense deposits in subendothelial and mesangial areas (Fig. 3.7). Vague wormy or microtubular substructure suggests a possible cryoglobulin component (Fig. 3.8). Cellular interposition is detected (Fig. 3.9), which refers to the interposition of cytoplasmic processes of mononuclear cells between the endothelial cell and the basement membrane. New basement material is present immediately under the swollen endothelial cells, resulting in the double contours visualized by light microscopy by silver stains [1].