Patient Story
A young Hispanic woman delivers a healthy baby boy. On the first postpartum day, she is sitting in the rocking chair after breastfeeding her son. Her doctor notes that she has melasma and asks her about it. She states that the hyperpigmented areas on her face have become darker during this pregnancy (Figure 197-1). She noted the dark spots started with her first pregnancy but they are worse this time. On physical examination, hyperpigmented patches are noted on the cheeks and upper lip (Figure 197-2). Although the patient hopes the pigment will fade, she does not want to treat the melasma at this time.
Introduction
Epidemiology
- It is a relatively common disorder that affects sun-exposed areas of skin, most commonly the face. It is believed to affect up to 75% of pregnant women.1
- It affects predominantly women (Figures 197-1, 197-2, and 197-3), with men accounting for only 10% of all cases. It is particularly prevalent in women of Hispanic, East Asian, and Southeast Asian origin (skin types IV to VI) and who live in areas of intense UV radiation exposure.1
- Melasma caused by pregnancy usually regresses within a year, but areas of hyperpigmentation may never completely resolve.2 It may increase with each subsequent pregnancy becoming more obvious.
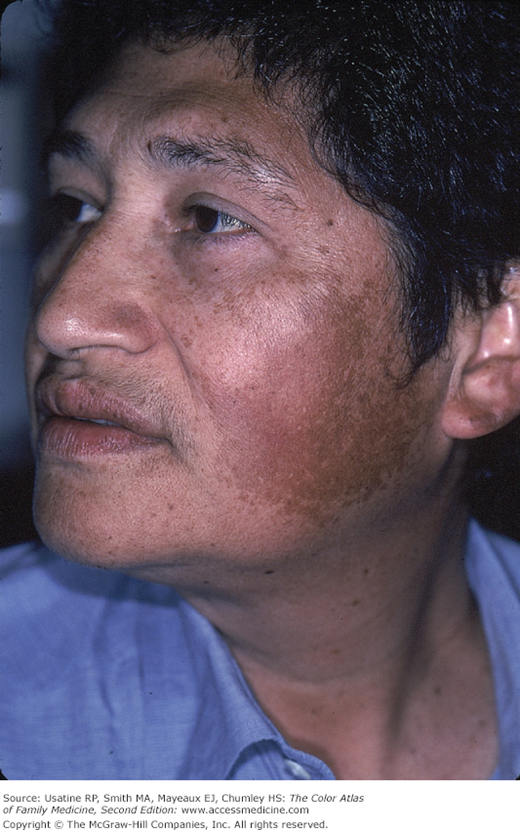
Figure 197-3
A 39-year-old Hispanic woman with melasma seeking treatment. She is disturbed by this dark color on her face. Note the hyperpigmentation reaches the eyebrows but does not cover the upper lip. She has not been pregnant for years and is not taking hormonal contraceptives. (Courtesy of Richard P. Usatine, MD.)
Etiology and Pathophysiology
- The precise cause of melasma has not been determined. Multiple factors have been implicated, including pregnancy, oral contraceptives, genetics, sun exposure, cosmetic use, thyroid dysfunction, and antiepileptic medications.3,4
- Women with melasma not related to pregnancy or oral contraceptive use may have hormonal alterations that are consistent with mild ovarian dysfunction.
- Melasma in men (Figure 197-4) shares the same clinical features as in women, but it is not known if hormonal factors play a role.5
Other factors associated with melasma include certain cosmetic ingredients (oxidized linoleic acid, salicylate, citral, preservatives) and certain antiepileptic drug. Some medications or topical preparations in combination with sun exposure worsen melasma.1
Risk Factors
A recent global survey of 324 women with melasma demonstrated that a combination of the known triggers, including pregnancy, hormonal birth control, family history, and sun exposure, affects onset of melasma.6
Diagnosis
The diagnosis of melasma is based upon clinical appearance. Affected patients exhibit splotchy areas of hyperpigmented macules on the face (Figures 197-1, 197-2, 197-3, and 197-4). In natural light, epidermal melasma appears light to dark brown, and the dermal pattern is blue or gray.
Melasma is divided into four clinical types:
Epidermal type—The hyperpigmentation is usually light brown, and Wood’s light enhances the color contrast between hyperpigmented areas and normal skin. It is the most common type, and it best responds to the use of depigmenting agents.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree