Melanoma, Superficial Spreading Type
Soheil Sam Dadras, MD, PhD
Nicole Carreau
Key Facts
Terminology
Most common variant of invasive melanoma
Clinical Issues
Most frequently occurs on back for males, legs for females
Broad macule with variegated colors
Irregular borders
Presence of papule/nodule may represent invasive component
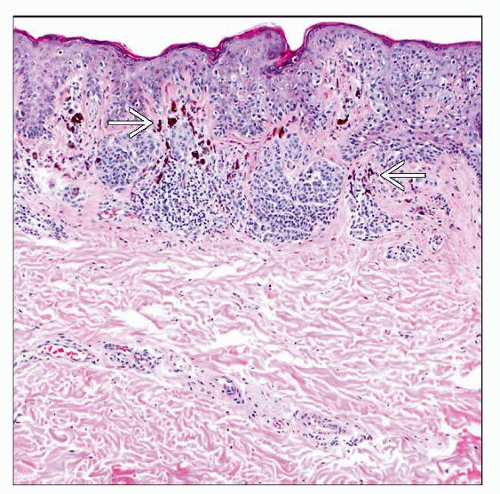
Microscopic Pathology
Proliferation of single atypical melanocytes involving both rete ridges and suprapapillary plates
Abundant pagetoid spread of atypical melanocytes located in spinous layer
Broad invasive front in which invasive dermal cells appear similar to overlying melanoma in situ (radial growth phase)
Highly atypical melanocytes form confluent nests or nodule in dermis
Lack of maturation of dermal component
Mitotic activity in deep dermal component
Dense but irregularly distributed inflammatory dermal infiltrate (mostly lymphocytes)
Asymmetrical distribution of melanin pigment
Top Differential Diagnoses
Severely dysplastic compound melanocytic nevus
Atypical Reed nevus
Epidermotropic metastatic melanoma
Paget disease
TERMINOLOGY
Abbreviations
Malignant melanoma, superficial spreading type (MMSST)
Definitions
Most common variant of invasive melanoma
Characterized histologically by lateral expansion of large dermal nests of atypical melanocytes, which appear similar to overlying melanoma in situ cells
CLINICAL ISSUES
Epidemiology
Incidence
6th most common cancer in USA with increasing incidence
Gender
Both men and women, but more common overall in men
Ethnicity
Typically persons with red hair and skin type I/II, but can occur in other ethnicities
Site
Varies according to gender, on the back (in men) and on the legs (in women)
Presentation
Large dark brown macule (2.5 cm is average size)
Variegated color with shades of tan, brown, black, blue-black, red (inflammation or vascular ectasia), gray and white (zones of regression)
Irregular borders
Presence of distinctive nodule can signify vertical growth phase
Treatment
Surgical approaches
Complete excision with clear margins
Peripheral margins are determined by depth of invasion (Breslow depth)
Prognosis
Varies according to Breslow depth, ulceration, and mitotic index
2010 AJCC criteria for determining prognosis
MACROSCOPIC FEATURES
Size
Typically > 1 cm in diameter
MICROSCOPIC PATHOLOGY
Histologic Features
Lateral expansion of large nests of atypical melanocytes in both epidermis and dermis, i.e., radial growth phase
Proliferation of single atypical melanocytes involving both rete ridges and suprapapillary plates
Abundant pagetoid spread of atypical melanocytes located in spinous layer
Irregular distribution of nests, which can be confluent with indented borders
Large artifactual clefts between nests and epidermis above
Highly atypical melanocytes form confluent nests or nodule in dermis
Nuclear to cytoplasmic ratio does not change with increasing dermal depth, i.e., dermal melanocytes fail to mature with increasing depth in dermis
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree