Patient Stories
A 40-year-old woman noticed a new dark spot on her neck (Figure 172-1). On examination the spot was 8 mm in its longest diameter, was asymmetrical with irregular borders, and had variation in color. A scoop shave biopsy demonstrated melanoma in situ. The spot was excised with 0.5 cm margins and no residual tumor was found in the excised ellipse. She has a near 100% chance of complete cure.
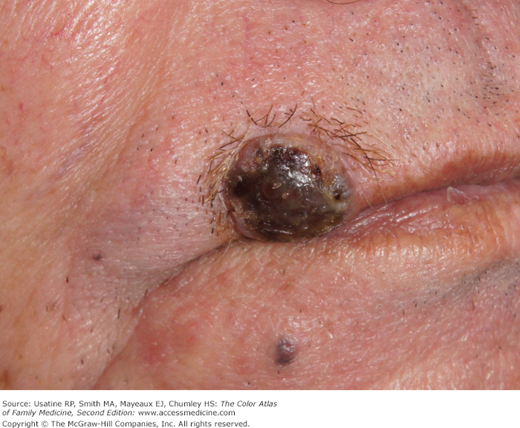
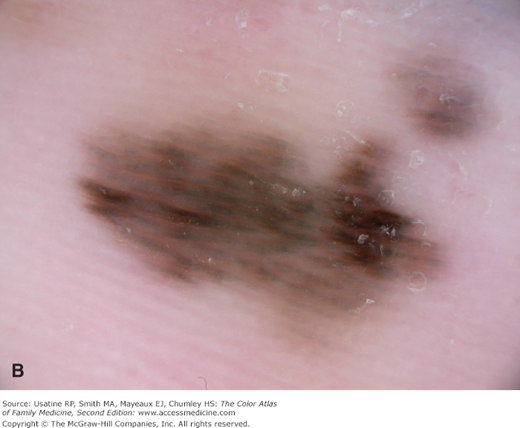
The wife of a 73-year-old man noticed that a “mole” on his back was enlarging and bleeding. (Figure 172-2). It had been there for years. Even though a year earlier a doctor had told him not to worry about it, his wife sent him to have it rechecked. Figure 172-2B shows a close-up of the pigmented lesion showing ulceration and bleeding. An elliptical excision was performed and the tissue appeared to be a nodular melanoma with dark pigment into the subcutaneous fat (Figure 172-2C). Histology revealed a nodular melanoma with a Breslow depth of 22 mm. The patient was referred to surgical and medical oncology. He underwent wide excision with 2-cm margins and a sentinel lymph node biopsy. The sentinel node was positive and further nodal dissection showed a total of another 4 axillary lymph nodes positive (1 on right and 3 on left). The lymph nodes on the left were black and enlarged. No distant metastases were found. Because more than 2 regional nodes were macroscopically positive, he was stage IIIC. He received radiation treatment to the original site and both axillae. Despite advances in targeted chemotherapy and immunotherapy, his prognosis was poor.
Figure 172-2
A. A 73-year-old man presents with bleeding “mole” on his back. Elliptical excision demonstrates this to be a nodular melanoma of 22-mm depth. B. Closeup of the nodular melanoma showing it to be thick with ulcerations and bleeding. C. Nodular melanoma after initial resection showing dark pigment into the subcutaneous fat. The Breslow depth is 22 mm with Clark level V. (Courtesy of Richard P. Usatine, MD.)
Introduction
Melanoma is the third most common skin cancer and the most deadly. The incidence of melanoma and the mortality from it are rising. Most lesions are found by clinicians on routine examination. When discovered early, surgical treatment is almost always curative. However, deeper lesions are prone to metastasize and have a much poorer prognosis. New therapies directed at the known gene changes in melanoma are beginning to show some promise, but widespread benefits of this research are still far off.
Epidemiology
- In 2012, an estimated 76,250 individuals will be diagnosed with melanoma of the skin and 9180 individuals will die from metastatic disease—or about 1 every hour.1
- Melanoma incidence has increased in every age group and in every thickness over the course of 1992 to 2006 among non-Hispanic whites, with death rates increasing in those older than age 65 years.2
- Incidence continues to increase worldwide at approximately 4% to 8% per year.3
- In the United States, the death rate for melanoma is decreasing among persons younger than age 65 years.2
- Deaths from thin melanomas account for more than 30% of total deaths.
- The lifetime risk of developing melanoma is 1 in 55 for men and 1 in 36 for women.1
Risk Factors
Risk factors can be broadly thought of as genetic risks, environmental risks, and phenotypic risks arising from a combination of genetic and environmental risks. For example, a fair-skinned child (genetic risk) who gets a sunburn (environmental) is much more likely to develop freckles (phenotypic) and melanoma.
- Exposure to sunlight.
- History of sunburn doubles the risk of melanoma and is worse at a young age.
- Living closer to the equator.
- Indoor tanning.
- History of immunosuppression.
- Higher socioeconomic status (likely associated with more frequent opportunity for sunburns).
- Fair skin, blue or green eyes, red or blonde hair.
- Male sex.
- Melanoma in a first-degree relative.
- History of xeroderma pigmentosa or familial atypical mole melanoma syndrome.
Diagnosis
Remember the ABCDE guidelines for diagnosing melanoma (Figure 172-3).4
- A = Asymmetry. Most early melanomas are asymmetrical: a line through the middle will not create matching halves. Benign nevi are usually round and symmetrical.
- B = Border. The borders of early melanomas are often uneven and may have scalloped or notched edges. Benign nevi have smoother, more even borders.
- C = Color variation. Benign nevi are usually a single shade of brown. Melanomas are often in varied shades of brown, tan, or black, but may also exhibit red, white, or blue.
- D = Diameter greater than or equal to 6 mm. Early melanomas tend to grow larger than most nevi. (Note: Congenital nevi are often large.)
- E = Evolving. Any evolving or enlarging nevus should make you suspect melanoma. Evolving could be in size, shape, symptoms (itching, tenderness), surface (especially bleeding), and shades of color.
- A prospective controlled study compared 460 cases of melanoma with 680 cases of benign pigmented tumors and found significant differences for all individual ABCDE criteria (p <0.001) between melanomas and benign nevi.4
- Sensitivity of each criterion: A 57%, B 57%, C 65%, D 90%, E 84%; specificity of each criterion: A 72%, B 71%, C 59%, D 63%, E 90%.4
- Sensitivity of ABCDE criteria varies depending upon the number of criteria needed: using 2 criteria it was 89.3%; with 3 criteria, it was 65.5%. Specificity was 65.3% using 2 criteria and 81% using 3.4
- The number of criteria present was different between benign nevi (1.24 ± 1.26) and melanomas (3.53 ± 1.53; p <0.001). Unfortunately, no significant difference was found between melanomas and atypical nevi.4
There are 4 major categories of melanomas. With the exception of nodular melanoma, the growth patterns of the 3 other subtypes are characterized by a radial growth phase prior to dermal invasion. At the present time, the thickness of the lesion histologically regardless of the morphologic type is used to stage the tumor and assess prognosis. In the future, molecular analysis may allow more accurate risk stratification.5 Here are the major categories of melanomas:
Superficial spreading melanoma is the most common type, representing 70% of all melanoma (Figures 172-3, 172-4, 172-5, and 172-6). This melanoma has the radial growth pattern before dermal invasion occurs. The first sign is the appearance of a flat macule or slightly raised discolored plaque that has irregular borders and is somewhat geometrical in form. The color varies, with areas of tan, brown, black, red, blue, or white. These lesions can arise in an older nevus. The melanoma can be seen almost anywhere on the body, but is most likely to occur on the trunk in men, the legs in women, and the upper back in both. Most melanomas found in the young are of the superficial spreading type.5
Nodular melanoma occurs in 15% to 30% of cases (Figures 172-2, 172-7, 172-8, and 172-9).5 It is usually invasive at the time it is first diagnosed, and the malignancy is recognized when it becomes a bump. The color is most often black, but occasionally is blue, gray, white, brown, tan, red, or nonpigmented. The nodule in Figure 172-9 is multicolored.
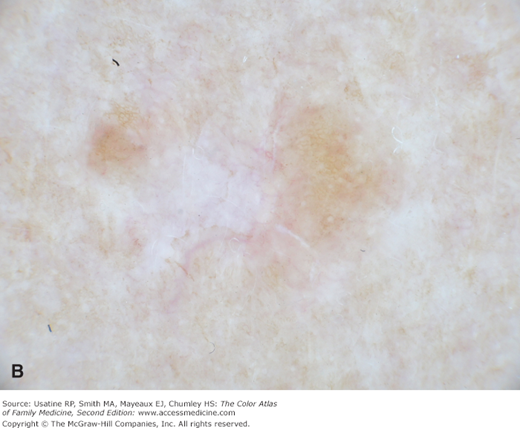
Lentigo maligna melanoma occurs in 4% to 15% of cutaneous melanoma.4 It is similar to the superficial spreading type and appears as a flat or mildly elevated mottled tan, brown, or dark brown discoloration. This type of melanoma is found most often in the elderly and arises on chronically sun-exposed, damaged skin on the face, ears, arms, and upper trunk. These account for most melanomas on the face. The average age of onset is 65 years and it grows slowly over 5 to 20 years. The precursor lesion, lentigo maligna, goes on to melanoma in approximately 5% of cases. The in situ precursor lesion is usually larger than 3 cm in diameter and has existed for a minimum of 10 to 15 years (Figures 172-10 and 172-11) (see Chapter 168, Lentigo Maligna).5
Acral lentiginous melanoma is the least common subtype of melanoma (2% to 8%) cases in white people; however, it is the most frequent subtype found in African Americans (70%) and is also a frequent subtype in Asians (45%).5 It may occur under the nail plate or on the soles or palms (Figures 172-12, 172-13, 172-14, 172-15, and 172-16). This subtype often carries a worse prognosis because of delays in diagnosis. Subungual melanoma may manifest as diffuse nail discoloration or a longitudinal pigmented band within the nail plate. When subungual pigment spreads to the proximal or lateral nail fold, it is referred to as the Hutchinson sign, and is highly suggestive of acral lentiginous melanoma (Figure 172-14) (see Chapter 191, Pigmented Nail Disorders).
Figure 172-9
Raised, thick, nodular melanoma on the shoulder of a 37-year-old white woman with history of multiple sunburns from childhood. Note the multiple colors visible in the nodule. The Breslow depth is 8.5 mm with Clark level V. The sentinel node was negative and the patient underwent chemotherapy after wide excision. (Courtesy of Richard P. Usatine, MD.)
Less common types of melanomas include:
- Amelanotic melanoma (<5% of melanomas) is nonpigmented and appears pink or flesh-colored, often mimicking basal cell or squamous cell carcinoma or a ruptured hair follicle. Any of the 4 principal subtypes may present as an amelanotic variant, but nodular melanomas are highly represented. These may be intrinsically more aggressive and often present with a thicker Breslow depth than similarly pigmented melanomas (Figures 172-17, 172-18 and 172-19).6
- Other rare melanoma variants include (a) nevoid melanomas, (b) malignant blue nevus, (c) desmoplastic/spindled/neurotropic melanoma, (d) clear cell sarcoma (in fact a melanoma), (e) animal-type melanoma, (f) ocular melanoma, and (g) mucosal (lentiginous) melanoma.5