Chapter 31 • Antispasmodic/anticholinergic agents are also known as antimuscarinic drugs. The muscarinic nervous system is a subcategory of the anticholinergic nervous system. The other subcategory, the nicotinic nervous system, is seldom involved in drug actions. Anticholinergic agents decrease motility, relax smooth muscle tone in the GI tract, and decrease secretions. • Antispasmodics decrease GI motility by relaxing smooth muscle tone. These medications have anticholinergic properties; thus, they compete with acetylcholine for receptors at postganglionic fibers of the parasympathetic nervous system. • Dicyclomine has indirect and direct effects on the smooth muscle of the GI tract. It indirectly blocks acetylcholine receptor sites and directly antagonizes bradykinin and histamine in GI tract smooth muscle. Both of these actions help to relieve smooth muscle spasm. • Hyoscyamine, a belladonna alkaloid, inhibits the muscarinic actions of acetylcholine at postganglionic parasympathetic neuroeffector sites, including smooth muscle, secretory glands, and CNS sites. Thus, this drug has an effect on peripheral cholinergic receptors present in the smooth muscle of the GI tract. Specific anticholinergic responses are dose related. Low doses inhibit salivary and bronchial secretions and sweating. Next, pupil dilation and accommodation are affected, and heart rate is increased. Higher doses decrease motility in GI and urinary tracts, and then inhibit gastric acid. • Antidepressants (particularly the TCAs), 5-HT3 (alosetron), and misoprostol have been found to be helpful in some patients. Please see Chapter 47 on antidepressants for a discussion of these products. • The American Gastroenterological Association developed guidelines for the treatment of patients with IBS; these were revised in 2002. World Gastroenterology Organization Practice Guideline—Irritable Bowel Syndrome. See www.worldgastroenterology.org/irritable-bowel-syndrome.html. • American College of Gastroenterology Task Force on Irritable Bowel Syndrome: An evidence-based position statement on the management of irritable bowel syndrome, Am J Gastroenterol 104(Suppl 1):S1-S34, 2009. Likely to be beneficial are the following: • Antidepressants: Tricyclics and SSRIs have been shown to reduce symptoms; it is not clear whether this is a separate effect from the antidepressant effect. • Smooth muscle relaxants have been noted to improve symptoms. • TABLE 31-2 • A trade-off occurs between benefits and harms of all medications. • 5-HT3 receptor antagonist alosetron (Lotronex): This agent has improved symptoms in women with diarrhea-predominant IBS and has increased constipation. It may be associated with ischemic colitis. • Pharmacotherapy is based on severity and is targeted at specific symptoms. • All patients with alternating constipation/diarrhea: • Loperamide—short term; often used for breakthrough diarrhea • Antidepressants (TCAs)—long term • Alosetron (ordered by GI specialists) if resistant to all other interventions Diet with adequate fiber is the cornerstone of treatment. Amounts of fiber and fluid usually have to be increased. Fiber should be increased gradually to avoid bloating. (See Chapter 28 for a list of high-fiber foods.) The patient should drink 6 to 8 glasses of water a day. The patient should identify and eliminate foods that cause symptoms. Foods that commonly cause problems include raw fruits and vegetables, high-fat foods, beverages such as carbonated beverages, coffee and other forms of caffeine, red wine and beer, and artificial sweeteners such as fructose and sorbitol. Exclude lactose intolerance. Other important lifestyle changes include good bowel habits and exercise. See Chapter 28 for a discussion of bowel training. The best exercise is usually regular walking. • Cramping abdominal pain—antispasmodic (anticholinergic) medication, as needed, when symptoms are present shortly after a meal • Abdominal pain, frequent or severe—TCAs • Constipation—increase dietary fiber, laxatives • Diarrhea—antidiarrheals such as loperamide (Imodium); severe—alosetron (females only) may be considered • Painful symptoms and diarrhea—TCAs • Painful symptoms and constipation—SSRIs (conflicting efficacy) • Simethicone use for problems with gas, including explosive bowel movements, belching, or flatus • Lubiprostone and polyethylene glycol also used for IBS (see Chapter 28)
Medications for Irritable Bowel Syndrome and Other Gastrointestinal Problems
Class
Subclass
Generic Name
Trade Name
Antispasmodics/anticholinergics
dicyclomine hydrochloride ![]()
Bentyl
hyoscyamine sulfate
Levsin, NuLev
5-HT3 Receptor antagonists
alosetron
Lotronex
GI stimulants/prokinetic agents
metoclopramide ![]()
Reglan
Prostaglandins
misoprostol
Cytotec
Ulcerative colitis treatment
mesalamine
Asacol
sulfasalazine
Azulfidine
Locally acting agents
simethicone
Phazyme, Gas-X
sucralfate
Carafate
Gallstone-solubilizing agents
ursodiol
Actigall
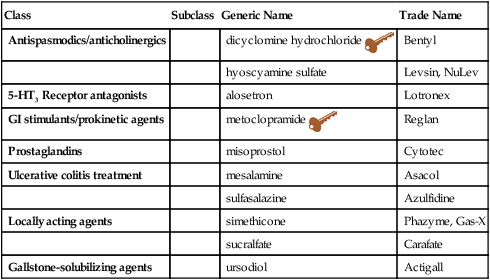
![]() Key drug. Key drug chosen because dicyclomine has a lower incidence of side effects.
Key drug. Key drug chosen because dicyclomine has a lower incidence of side effects.
Mechanism of Action
Treatment Principles
Standardized Guidelines for IBS
Evidence-Based Recommendations for IBS
![]() Psyllium fiber, certain antispasmodics, and peppermint oil are effective. See Table 31-2 for more on complementary and alternative therapies.
Psyllium fiber, certain antispasmodics, and peppermint oil are effective. See Table 31-2 for more on complementary and alternative therapies.
![]() Complementary and Alternative Products That May Have Interactions with Other Drugs
Complementary and Alternative Products That May Have Interactions with Other Drugs
Condition
Product
Comments
Irritable bowel
Cat’s claw
Potential interaction with anticoagulants, aspirin, antiplatelet agents. May stimulate immune system. May protect against GI damage from NSAIDs.
Flaxseed
May slow down absorption of oral medications or other nutrients if taken at the same time.
Grapefruit seed extract
Avoid concurrent administration of terfenadine, astemizole, cisapride; use other medications metabolized by the CYP 3A4 subsystem with caution.
Evening primrose
Potential interaction with anticoagulants, aspirin, NSAIDs, antiplatelet agents; phenothiazines used to treat schizophrenia
Peppermint
No known interactions
Gallbladder/gallstones
Milk thistle Artichoke Goldenseal
No reported toxicities with any of these products
Gallbladder disease
Milk thistle
Artichoke
No reported toxicities with either of these products
Cardinal Points of Treatment
Nonpharmacologic Treatment
Pharmacologic Treatment
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Medications for Irritable Bowel Syndrome and Other Gastrointestinal Problems
Only gold members can continue reading. Log In or Register to continue
