Mediastinoscopy
James Wiseman
Shanda Haley Blackmon
DEFINITION
Mediastinoscopy is the evaluation of the anterior mediastinum through endoscopic means.
Video mediastinoscopy is the current technique discussed in this chapter.
It remains the gold standard for mediastinal exploration in lung cancer staging and can be applied to the sampling of any tissue of the anterior mediastinum for diagnostic purposes.
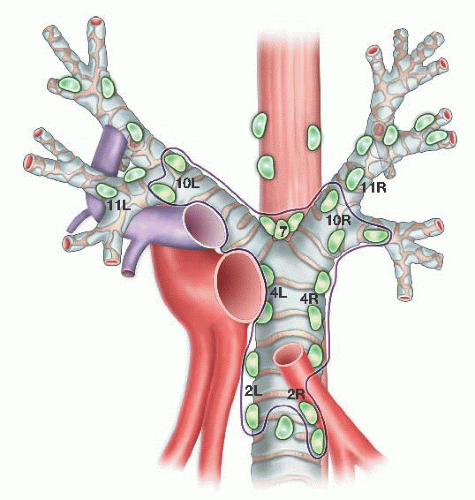
Through traditional video mediastinoscopy, levels 2, 4, 7, and 10 lymph nodes can be reached (FIG 1). Through an extended cervical mediastinoscopy (ECM), the paraaortic and aortopulmonary lymph nodes can be reached.
Additionally, but less frequently, mediastinoscopy can be used in the setting of mediastinal disease for therapeutic purposes.
IMAGING AND OTHER DIAGNOSTIC STUDIES
Patients being considered for mediastinoscopy frequently present following identification of either mediastinal or pulmonary pathology on plain film radiography. A minimum of two views is required to differentiate between abnormalities of the anterior, middle, and posterior mediastinum, including either a posteroanterior view or an anteroposterior projection and a lateral projection. Lymphadenopathy is rarely visible on plain films, typically necessitating the use of alternative imaging modalities in assessing for lymph node enlargement.
Computed tomography (CT) of the chest is a critical tool in the early evaluation of patients with known or suspected lung cancer or other diseases involving mediastinal structures. The primary use of CT is the radiographic visualization of abnormalities of the mediastinum (i.e., neoplasm, abscess, lymphadenopathy). In the setting of lung cancer, CT is most useful in identification of mediastinal adenopathy. Lymph nodes are considered to be positive if they demonstrate a short-axis diameter larger than 1 cm. Using this threshold, however, the negative predictive value (NPV) of CT scan ranges from 77% to 90%, with a positive predictive value (PPV) of 41% to 74%.1, 2, 3 Despite these limitations, the use of CT has allowed some centers to implement a selective approach to mediastinoscopy.
Considerable attention has been given to the use of positron emission tomography (PET) in the evaluation of primary mediastinal pathology and, in particular, assessment of the mediastinum for lymphadenopathy in the evaluation of the lung cancer patient. Several studies have reported NPV in excess of 95% with the use of PET to evaluate for metastatic disease to mediastinal lymph nodes.4, 5, 6 False-positive findings are frequent with PET, however, and the identification of PET-avid nodes demands confirmation.
SURGICAL MANAGEMENT
The most common indication for mediastinoscopy is for staging in the setting of lung cancer. Some institutions employ mediastinoscopy routinely in the evaluation of these patients. Others advocate for a selective approach, informed by the findings of other imaging modalities. In this setting, centrally located tumors, known as adenocarcinoma, nodes larger than 1 cm on CT scan, and PET-avid nodes should prompt the use of invasive means of obtaining tissue for diagnosis.
Mediastinoscopy is also a valuable diagnostic tool in the evaluation of nonneoplastic causes of mediastinal lymphadenopathy as well as other masses found in the mediastinum for which identification cannot be accomplished through noninvasive means.
Absolute contraindications to mediastinoscopy include innominate artery aneurysms and the presence of a tracheostomy.7
The presence of a thyroid goiter, depending on size, may present technical difficulties for the surgeon, and very large goiters may preclude performance of the procedure altogether.
Repeat mediastinoscopy, although challenging, is usually possible and safe.
Preoperative Planning
A complete history and physical, focusing specifically on previous mediastinal operations, should be obtained. Although prior mediastinal surgery (coronary artery bypass graft [CABG] surgery, esophagectomy, etc.) does not preclude mediastinoscopy, it is essential to be aware of such history during the planning phase.
All patients with planned mediastinoscopy should have coagulation studies done preoperatively. In general, a target international normalized ratio (INR) of 1.2 should be achieved to minimize risk of intraoperative and postoperative bleeding. Antiplatelet therapy should be stopped prior to an elective procedure such as mediastinoscopy.
Positioning
Following induction of general anesthesia, the patient is placed supine with the head close to the top edge of the operating table. The procedure can be facilitated through extension of the neck by placement of a rolled towel or beanbag device horizontally from shoulder to shoulder. Some patients may not tolerate complete neck extension due to prior cervical spine surgery or degenerative disease.
The entire neck and chest should be sterilely prepped and draped in the event that an emergent sternotomy is required to address intraoperative complications.
TECHNIQUES
INCISION
The typical location of the incision is centered along the midline, approximately 1 cm superior to the sternal notch. We favor a horizontal incision, with a length of approximately 1.5 to 2.5 cm (FIG 2).
The incision is carried through the platysma and subcutaneous tissue until the vertically oriented sternohyoid muscles are identified. The avascular plane separating these muscles can then be opened, revealing the underlying sternothyroid muscles.
The surgeon will occasionally encounter engorged anterior jugular veins or their tributaries at this level of the dissection. These represent a significant bleeding risk and can be ligated if hemorrhage is encountered or anticipated. Clips should be avoided as they are prone to dislodgement with advancement of the mediastinoscope.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree