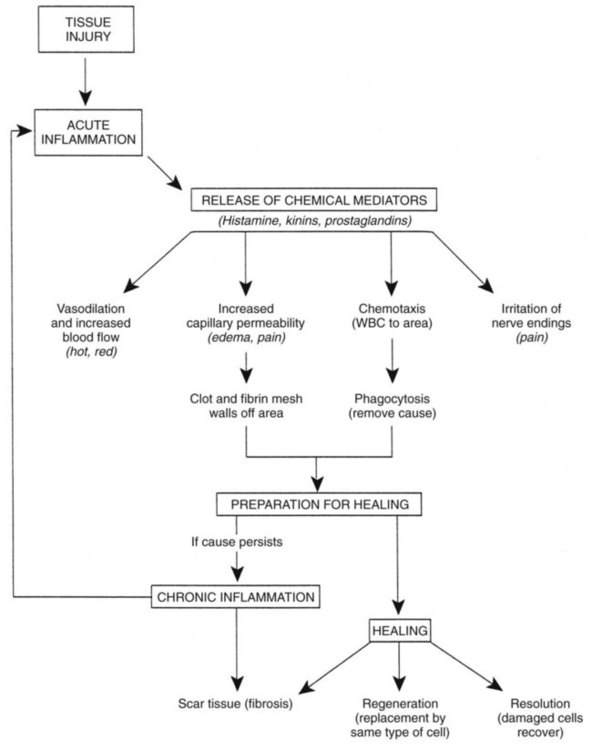
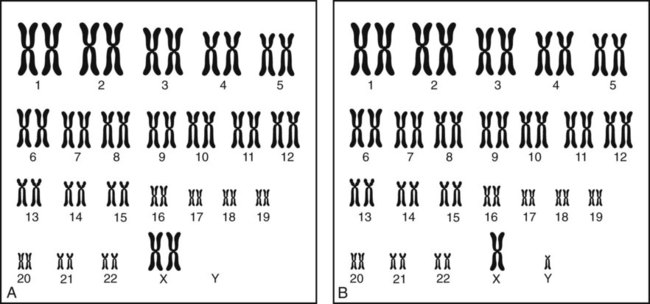
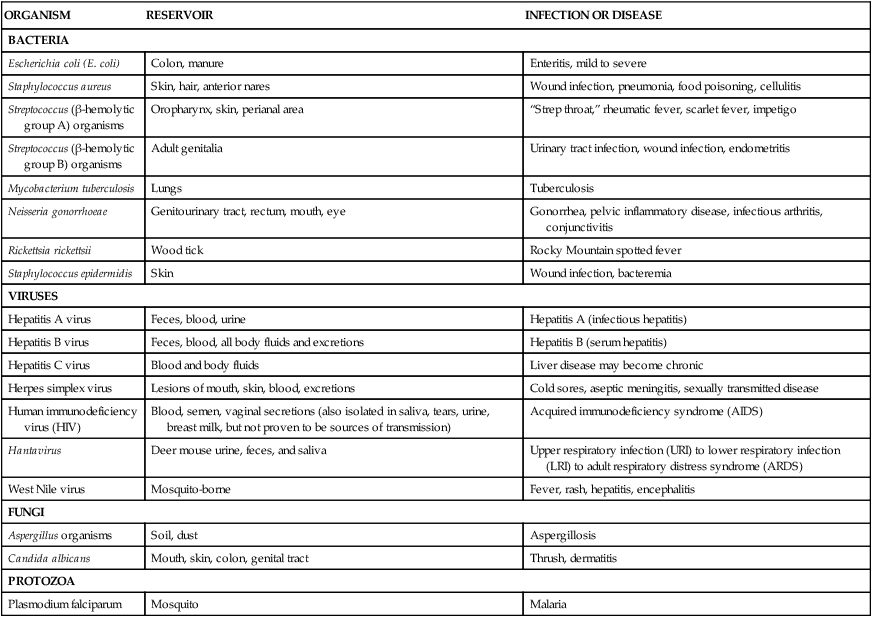
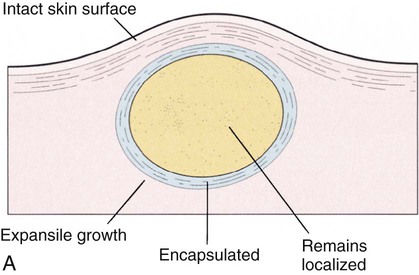
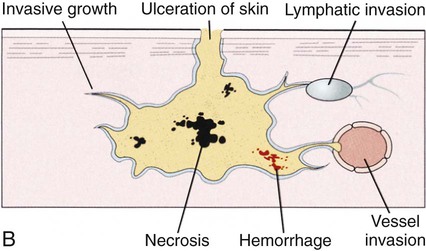
After studying Chapter 1, you should be able to: 1. Explain how a pathologic condition affects the homeostasis of the body. 2. Describe the difference between: Benign and malignant neoplasms 3. Identify the predisposing factors of disease. 4. Describe the ways in which pathogens may cause disease. 5. Track the essential steps in diagnosis of disease. 6. List the prevention guidelines for cancer. 7. Explain the inflammation response to disease. 8. Describe the hospice concept of care. 9. Name two ways an individual can practice positive health behavior. 10. Describe (a) the physiology of pain, (b) how pain may be treated, and (c) what is meant by referred pain. 11. Define the holistic approach to medical care. 12. Describe examples of nontraditional medical therapies. 13. Define integrative medicine. 14. Discuss the principles and goals of patient teaching. 15. List some health effects of exposure to secondhand tobacco smoke. Age. From complications during pregnancy and the postpartum period to maladies associated with aging, some increased risks of diseases are simply intrinsic to one’s stage in the human life cycle. Gender. Certain diseases are more common in women (e.g., multiple sclerosis and osteoporosis) and other disorders are more common in men (e.g., gout and Parkinson’s disease). Lifestyle. Occupation, habits, or one’s usual manner of living can have negative cumulative effects that can threaten a person’s health. It is possible to alter some known risk factors associated with lifestyle, thereby promoting health instead of predisposing one to disease; examples include smoking, excessive drinking of alcohol, risky sexual behavior, poor nutrition, lack of exercise, and certain psychological stressors. Environment. Air and water pollution is considered a major risk factor for illnesses such as cancer and pulmonary disease. Poor living conditions, excessive noise, chronic psychological stress, and a geographic location conducive to disease proliferation also are environmental risk factors. Heredity. Genetic predisposition (inheritance) currently is considered a major risk factor. Family histories of coronary disease, cancer, certain arthritic conditions, and renal disease are known hereditary risk factors. Many other genetic links to diseases are rapidly being discovered. Hereditary factors in disease that appear regularly in successive generations are likely to affect males and females equally. Hereditary or genetic diseases often develop as a result of the combined effects of inheritance and environmental factors. Examples are mental illness, cancer, hypertension, heart disease, and diabetes. Some evidence shows that smoking, a sedentary lifestyle, and a diet high in saturated fat, combined with a positive family history, compound a person’s risk for heart disease and cancer. Schizophrenia may result from a combination of genetic predisposition and numerous psychological and sociocultural causes. Acute inflammation, an exudative response, attempts to wall off, destroy, and digest bacteria and dead or foreign tissue. Vascular changes allow fluid to leak into the site; this fluid contains chemicals that permit phagocytic activity by white blood cells. The process prevents the spread of infection through antibody action and other chemicals released by cells with more specific immune activity. After the mechanisms of inflammation have contained the insult and “cleaned up” the damaged area, repair and replacement of tissue can begin (Figure 1-1). A normal inflammatory response can be inhibited by immune disorders, chronic illness, or the use of certain medications, especially long-term steroid therapy. The sources of infection can be endogenous (originating within the body) or exogenous (originating outside the body). Modes of transmission of pathogenic organisms are direct or indirect physical contact, inhalation or droplet nuclei, ingestion of contaminated food or water, or inoculation by an insect or animal. Pathogenic agents include bacteria, viruses, fungi, and protozoa (Table 1-1). E1-2 TABLE 1–1 Common Pathogens and Some Infections or Diseases That They Produce Modified from Potter P, Perry A: Fundamentals of nursing: concepts, process, and practice, ed 6, St Louis, 2006, Mosby. Every cell in the body is coded with genetic information arranged on 23 pairs of chromosomes; one chromosome from each pair is inherited from the father and the other from the mother. The X and Y chromosomes are known as the sex chromosomes, whereas the remaining 22 pairs are called autosomes. Each cell in an individual’s body contains the same chromosomes and genetic code (genotype). A karyotype is an ordered arrangement of photographs of a full chromosome set (Figure 1-2). Genes, the basic units of heredity, are small stretches of a DNA (deoxyribonucleic acid) molecule, situated at a particular site on a chromosome. The main modes of inheritance for genetic diseases are as follows: The following examples of genetic abnormalities are discussed in this book: Cancer, a leading cause of death in the United States, refers to a group of diseases characterized by uncontrolled cell proliferation. This abnormal growth leads to the development of tumors or neoplasms, a relentlessly growing mass of abnormal cells that proliferates at the expense of the healthy organism. Tumors are characterized as malignant or benign and according to the cell type and tissue of origin (Tables 1-2 and 1-3). Some of the main general types of cancer are carcinoma, cancer of the epithelial cells; sarcoma, cancer of the supportive tissues of the body, such as bone and muscle; lymphoma, cancer arising in the lymph nodes and tissues of the immune system; leukemia, cancer of blood cell precursors; and melanoma, cancer of the melanin-producing cells of the body. TABLE 1–2 Comparison of Benign and Malignant Tumors TABLE 1–3 Classification of Neoplasms by Tissue of Origin From Black JM, Matassarin-Jacobs E: Medical-surgical nursing, ed 6, Philadelphia, 2001, Saunders. Cancer is actually many different diseases with numerous causes. Cancer may be caused by both external exposure to carcinogens (chemicals, radiation, and viruses) and internal factors (hormones, immune conditions, and inherited mutations). Ten years or longer may pass between exposures or mutations and the onset of detectable cancer. Cancer can develop in anyone, but the frequency increases with age. Figure 1-3 shows the leading sites of cancer incidence and death. • Consume a diet rich in fruits, vegetables, and whole grains and low in saturated and trans fats • Eliminate active and passive exposure to cigarette smoke • Limit skin exposure to sunlight • Avoid excessive exposure to radiation and radon • Avoid chemical agents known to be carcinogenic • Protect against sexually transmitted infections, including getting the HPV vaccine Although a number of different staging systems exist, the majority of cancers use a TNM system. TNM staging assesses the neoplasm in three different areas: the size or extent of the primary tumor (T), the extent of regional lymph node involvement by the tumor (N), and the number of distant metastases (M). Once all three parameters are defined, they are combined to assign a stage number of I, II, III, or IV to the cancer. One is an early stage tumor and carries the best prognosis, whereas IV is the most advanced stage. Within each stage, subcategories are defined (Ia, Ib, etc.) to further aid in treatment planning and facilitation of communication between institutions and physicians. See Table 1-4 for an example of staging. TABLE 1–4 Melanoma Staging System of the American Joint Committee on Cancer
Mechanisms of Disease, Diagnosis, and Treatment
Pathology at First Glance
Mechanisms of Disease
Predisposing Factors
Inflammation and Repair
Infection
ORGANISM
RESERVOIR
INFECTION OR DISEASE
BACTERIA
Escherichia coli (E. coli)
Colon, manure
Enteritis, mild to severe
Staphylococcus aureus
Skin, hair, anterior nares
Wound infection, pneumonia, food poisoning, cellulitis
Streptococcus (β-hemolytic group A) organisms
Oropharynx, skin, perianal area
“Strep throat,” rheumatic fever, scarlet fever, impetigo
Streptococcus (β-hemolytic group B) organisms
Adult genitalia
Urinary tract infection, wound infection, endometritis
Mycobacterium tuberculosis
Lungs
Tuberculosis
Neisseria gonorrhoeae
Genitourinary tract, rectum, mouth, eye
Gonorrhea, pelvic inflammatory disease, infectious arthritis, conjunctivitis
Rickettsia rickettsii
Wood tick
Rocky Mountain spotted fever
Staphylococcus epidermidis
Skin
Wound infection, bacteremia
VIRUSES
Hepatitis A virus
Feces, blood, urine
Hepatitis A (infectious hepatitis)
Hepatitis B virus
Feces, blood, all body fluids and excretions
Hepatitis B (serum hepatitis)
Hepatitis C virus
Blood and body fluids
Liver disease may become chronic
Herpes simplex virus
Lesions of mouth, skin, blood, excretions
Cold sores, aseptic meningitis, sexually transmitted disease
Human immunodeficiency virus (HIV)
Blood, semen, vaginal secretions (also isolated in saliva, tears, urine, breast milk, but not proven to be sources of transmission)
Acquired immunodeficiency syndrome (AIDS)
Hantavirus
Deer mouse urine, feces, and saliva
Upper respiratory infection (URI) to lower respiratory infection (LRI) to adult respiratory distress syndrome (ARDS)
West Nile virus
Mosquito-borne
Fever, rash, hepatitis, encephalitis
FUNGI
Aspergillus organisms
Soil, dust
Aspergillosis
Candida albicans
Mouth, skin, colon, genital tract
Thrush, dermatitis
PROTOZOA
Plasmodium falciparum
Mosquito
Malaria
Genetic Diseases
Cancer
CHARACTERISTICS
BENIGN
MALIGNANT
Mode of growth
Relatively slow growth by expansion; encapsulated; cells adhere to each other
Rapid growth; invades surrounding tissue by infiltration
Cells under microscopic examination
Resemble tissue of origin; well differentiated; appear normal
Do not resemble tissue of origin; vary in size and shape; abnormal appearance and function
Spread
Remains localized
Metastasis; cancer cells carried by blood and lymphatics to one or more other locations; secondary tumors occur
Other properties
No tissue destruction; not prone to hemorrhage; may be smooth and freely movable
Ulceration and/or necrosis; prone to hemorrhage; irregular and less movable
Recurrence
Rare after excision
A common characteristic
Pathogenesis
Symptoms related to location with obstruction and/or compression of surrounding tissue or organs; usually not life-threatening unless inaccessible
Cachexia; pain; fatal if not controlled
TISSUE OF ORIGIN
BENIGN
MALIGNANT
Connective tissue
Sarcoma
Embryonic fibrous tissue
Myxoma
Myxosarcoma
Fibrous tissue
Fibroma
Fibrosarcoma
Adipose tissue
Lipoma
Liposarcoma
Cartilage
Chondroma
Chondrosarcoma
Bone
Osteoma
Osteogenic sarcoma
Epithelium
Carcinoma
Skin and mucous membrane
Papilloma
Squamous cell carcinoma
Glands
Basal cell carcinoma
Transitional cell carcinoma
Adenoma
Adenocarcinoma
Cystadenoma
Cystadenocarcinoma
Pigmented cells (melanocytes)
Nevus
Malignant melanoma
Endothelium
Endothelioma
Blood vessels
Hemangioma
Hemangioendothelioma
Hemangiosarcoma
Kaposi sarcoma
Lymph vessels
Lymphangioma
Lymphangiosarcoma
Lymphangioendothelioma
Bone marrow
Multiple myeloma
Ewing sarcoma
Leukemia
Lymphoid tissue
Malignant lymphoma
Lymphosarcoma
Reticulum cell sarcoma
Muscle tissue
Smooth muscle
Leiomyoma
Leiomyosarcoma
Striated muscle
Rhabdomyoma
Rhabdomyosarcoma
Nerve tissue
Nerve fibers and sheaths
Neuroma
Neurinoma
(Neurilemoma)
Neurogenic sarcoma
Neurofibroma
(Neurofibrosarcoma)
Ganglion cells
Ganglioneuroma
Neuroblastoma
Glial cells
Glioma
Glioblastoma
Meninges
Meningioma
Malignant meningioma
Gonads
Dermoid cyst
Embryonal carcinoma
Embryonal sarcoma
Teratocarcinoma
PRIMARY TUMOR (pT)
pTX
Primary tumor cannot be assessed.
pTO
No evidence of primary tumor
pTis
Melanoma in situ (atypical melanotic hyperplasia, severe melanotic dysplasia), not an invasive lesion (Clark’s Level I)
pT1
Tumor 0.75 mm or less in thickness and invades the papillary dermis (Clark’s Level III)
pT3
Tumor more than 1.5 mm but not more than 4 mm in thickness and/or invades the reticular dermis (Clark’s Level IV)
pT3a
Tumor more than 1.5 mm but not more than 3 mm in thickness
pT3b
Tumor more than 3 mm but not more than 4 mm in thickness
pT4
Tumor more than 4 mm in thickness and/or invades the subcutaneous tissue (Clark’s Level V) and/or satellite(s) within 2 cm of the primary tumor
pT4a
Tumor more than 4 mm in thickness and/or invades the subcutaneous tissue
pT4b
Satellite(s) within 2 cm of primary tumor
LYMPH NODE (N)
NX
Regional lymph nodes cannot be assessed.
NO
No regional lymph node metastasis
N1
Metastasis 3 cm or less in greatest dimension in any regional lymph nodes
N2
Metastasis more than 3 cm in greatest dimension in any regional lymph node(s) and/or in-transit metastasis
N2a
Metastasis more than 3 cm in greatest dimension in any regional lymph node(s)
N2b
In-transit metastasis
N2c
Both (N2a and N2b)
DISTANT METASTASIS (M)
MX
Presence of distant metastasis cannot be assessed.
MO
No distant metastasis
M1
Distant metastasis
M1a
Metastasis in skin or subcutaneous tissue of lymph node(s) beyond the regional lymph nodes
M1b
Visceral metastasis
STAGE GROUPING
Stage I
pT1, pT2
NO
MO
NO
MO
Stage II
pT3
NO
MO
Stage III
pT4, Any pT
NO
MO
N1, N2
MO
Stage IV
Any pT
Any N
M1 ![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree