9
Chapter Outline
| Web Toolkit available at www.ashp.org/ambulatorypractice |
Chapter Objectives
1. Develop a plan for growth for your clinical services by analyzing the demand and need for services.
2. Contribute to practice-based research to expand knowledge regarding ambulatory care pharmacy practice.
3. Create an environment conducive to training future ambulatory care pharmacy practitioners, including postgraduate year 1 and postgraduate year 2 residents.
4. Anticipate changes in health care delivery and financing that may impact ambulatory care pharmacy practice.
Introduction
Building a successful ambulatory care practice requires more than a personal commitment to helping patients achieve optimal health outcomes. It requires a long-term vision and a strategic plan. You’ll soon discover (if you haven’t already) that the medication-related needs of the patients in your practice are far more than you or even a small team of ambulatory care pharmacists can handle. Once the value of your services has been firmly established, you’ll likely become overwhelmed by the patient volume, and you’ll find new medication-related problems that need attention. And just when you think you’ve got it all figured out, things will change. No one can predict the future, but you can be certain that the world around you won’t remain stagnant. New medications and technologies will bring new challenges. And the need for your services will grow and shift over time. Changes in health care financing may lead to a major transformation in the health care system as monetary incentives encourage health systems to adopt new methods, engage in new activities, and set new priorities. And there will be a continual need for new knowledge and understanding as we uncover new problems and attempt to find new solutions.
In this chapter we explore how to maximize your practice by
- growing and expanding your services,
- contributing to our knowledge,
- training the next generation of ambulatory care specialists,
- anticipating the future, and
- planning strategically for long-term success (Figure 9-1).
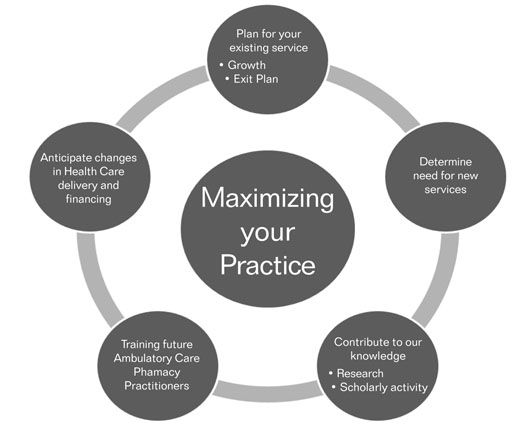
Figure 9-1. Maximizing Your Practice
Planning for Growth
CASE
You are now a board-certified ambulatory care pharmacist and have been working for Dr. Busybee for 3 years. The pharmacotherapy consult service you created initially to manage diabetes and anticoagulation patients is growing rapidly. You are now working at the clinic 5 days a week. Initially, referrals to the pharmacotherapy consult service came from Dr. Busybee, but soon word spread among the other providers regarding the availability and success of your service. In fact the referrals are now expanding to hypertension and dyslipidemia, as your work with diabetic patients has demonstrated your ability to assist with medication management of these conditions. Your growth has been fast, and you are struggling to meet the demands of the new, more complex patient health concerns. The following table illustrates the growth of the service and the change in its case mix.
| 36 Months Ago | 24 Months Ago | 12 Months Ago | Now |
| Total number of patient encounters (per month): | |||
| 200 | 325 | 400 | 550 |
| New referrals (per month): | |||
| 37 | 71 | 80 | 99 |
| INDICATIONS FOR REFERRAL | |||
| Anticoagulation | |||
| VTE prophylaxis (Ortho): | |||
| 20 | 59 | 72 | 70 |
| Atrial fibrillation: | |||
| 15 | 50 | 82 | 90 |
| VTE treatment: | |||
| 30 | 42 | 49 | 73 |
| Prosthetic heart valve: | |||
| 3 | 6 | 14 | 32 |
| Medication Management | |||
| Diabetes: | |||
| 2 | 8 | 15 | 20 |
| Hypertension: | |||
| 0 | 0 | 5 | 10 |
| Dyslipidemia: | |||
| 0 | 0 | 3 | 8 |
| VTE = venous thromboembolism | |||
With the growth and expansion of your service, you have updated your collaborative practice agreement to include hypertension and dyslipidemia. Additionally, the physicians are requesting your assistance in medication reconciliation for all patients seen in the office who were recently discharged from a hospital or extended care facility. Despite the growth, the majority of your practice still remains anticoagulation management. However, an increasing number of patients are being initiated or converted to the new oral anticoagulants for atrial fibrillation and postoperative orthopedic procedures. You have a sense that anticoagulation referrals seem to be declining, and there is more and more interest in your assistance with patients with other disease states. You have the following issues and concerns:
• New oral anticoagulation therapies will change patient management and monitoring requirements. Dr. Busybee and his partners are interested in converting appropriate patients to the new oral anticoagulation medications. Initially, the use of the new oral anticoagulants may be limited by cost and the need to gain experience with the new medications in your population, but you anticipate that they will be prescribed more often over the next year. How should you approach and plan for this anticipated change? Should you ignore, reject, or accept these new drugs?
• Continued growth of the service is unsustainable. With the increased referrals of more complex non-anticoagulation patients, you are finding you are becoming increasingly busy. You believe that you have reached the clinic’s capacity with a single practitioner. You currently have a very limited amount of time for other responsibilities (e.g., administrative tasks). Indeed, you often work late to catch up on paperwork and make phone calls to patients. Moreover, finding coverage during periods of your absence (e.g., vacations, illness, and professional meetings) has become problematic. Although the number of new referrals continues to increase overall, the number of patients with long-term indications for warfarin therapy has decreased slightly. How should you approach and plan for this issue? Should you figure the decrease in patients on warfarin will offset the increase in other patient referrals? In the meantime how do you handle how busy you are? Are you expanding too quickly?
When you establish a new practice, it is certainly rewarding to finally “open” the clinic and begin to provide care for patients. Since provision of patient care was your ultimate goal and may be what most interests you in your job, it may be tempting to consider your task of building a successful practice complete. However, clinicians who fail to maintain their focus on managing the practice may find their practice faltering or exceeding their capacity.
When building your infrastructure, you thought carefully about determining not only the appropriate services to provide but also the resource needs (see Chapter 2). In determining the number of full-time equivalent (FTE) pharmacists needed to establish the service, you considered several factors, including the number of hours per day and days per week the service would be available, the predicted patient volume, the distribution of face-to-face patient visits and telephone encounters, and the availability of support staff. As your practice grows, it is important to monitor for changes in your original plan. Has your distribution of face-to-face visits increased over the projected plan? What about the volume of new referrals? For example, you may follow 100 patients, but there is 20% turnover every quarter as patients meeting their treatment goals are discharged and new referrals are accepted. Compared to a stable practice of 100 patients with few new referrals, this means substantially more new patient visits, which are more time consuming. (Updated Resources and Reimbursement Worksheet)![]()
 | Reevaluate your service and resource needs, including patient volume and staffing levels, at regular time intervals. |
It is important to set aside some time at regular intervals, quarterly or semiannually, to critically examine the trends and shifts in your practice. This will prevent any gradual creeps in service volume from causing a staffing crisis. The most difficult time to deal with these issues is when you are busy caring for your patients, leaving little time to devote to administrative tasks. Alternatively, early identification of a fall in demand for your services should prompt you to perform a needs assessment and develop new services in areas of need rather than face scrutiny from administration regarding overstaffing. Since you should be reviewing your services on a quarterly or semiannual basis for quality assessment (Chapter 7, Quality Assurance for Ambulatory Patient Care), this is an ideal time to look at the overall needs of the service. Your quality report should contain information on service activity, such as the number of patients and the number of referrals as well as the number and type of patient encounters. Use this as an opportunity to think about what the numbers mean. Has your total patient load increased? What about the nature and type of patient encounters? (Example Measures to Examine Trends in Practice) ![]()
In addition to developing a set timeline for evaluating increases and decreases in service demand, it is important to consider your business plan. You should establish benchmark metrics that prompt staffing adjustments. For example, build into your business plan that when you reach 90% of capacity, the criteria and process to hire additional staff will already be established. Allow time for necessary administrative approvals for new positions, recruitment, hiring, and training new members of the team. Depending on the administrative structure at your institution, this may take 6 months or more. If your service is part-time, for example an anticoagulation clinic offered 2 days per week, establish a benchmark for when a third day will be added. Responsibilities of the pharmacist on service will need to be shifted to accommodate the added workload, and ideally this growth should be anticipated. If additional staff are not an option due to resource constraints, consider capping or closing the service at a prespecified number of patients.
You may even be able to anticipate swings in patient-care volume. Take a step back from your practice and think about your health system and changes in the local environment. If a large cardiology group is added to a health system, an antithrombosis clinic may experience a rapid increase in patient volume. If a nurse practitioner is hired by a key endocrinology group to assist in patient management, your diabetes service may experience a decline in referrals. Furthermore, if your health system decides to no longer accept a certain insurance plan and a large number of your patient population happens to have this plan, how will this impact your patient volume?
Not only does the volume of patient care encounters need to be considered in workload planning and resource needs, but non-patient care activities of the ambulatory care specialist must be considered in a growing service. Some of these elements are directly related to the patient care provided. In your original estimation of resource needs, did you adequately account for these elements, or do you find they are taking more time? You may have underestimated the amount of time administrative tasks related to patient care takes, and clinicians cannot be expected to provide direct patient care 40 hours per week. Time needs to be set aside for administrative tasks related to patient care, such as phone calls from patients with clinical concerns, rescheduling patients and contacting patients who do not show for appointments, coordinating care, and documentation. If you find this was not accounted for properly in your original plan, it may be worthwhile to track the time you devote to these ancillary tasks as your practice grows. A 1- to 2-week self-study tracking the number of hours devoted to non-patient care or the number of phone calls may help you get a better estimate of resource needs related to these tasks. This objective information will help you to rework your resource allocation and perhaps help you to justify adjusting clinic hours downward or hiring support staff for administrative tasks. (Tracking Tool for Non-patient Activities) ![]()
 | Non-patient care related activities must be considered in a growing service. |
Since you first estimated your resource needs, the scope of non-patient care services may have shifted in your practice. Successful ambulatory care practices often become training sites for pharmacy students and residents. Leaders in the health care organization may look to a successful ambulatory care practitioner to fulfill key roles on committees within the organization or to serve as an advisor in a specific therapeutic area. For example, a clinician in a diabetes clinic may be asked to provide an assessment of a new drug being considered for inclusion on a formulary or to provide staff in-services. You may be extensively involved in developing quality metrics and reporting for your practice, as outlined in Chapter 7. If you are an ambulatory care pharmacy specialist, consider how your role has changed since the clinical service was developed and the initial needs assessment was outlined. Are you more or less involved in committee work? Do you chair any committees? Have you become involved in student precepting or resident training? Do you serve as a residency program director or teach in the classroom? How much of your time do you devote to quality reporting or scholarly activity? If you are the manager for a group of clinical pharmacy specialists, have your specialists become more engaged in these elements of pharmacy practice?
CASE
You face a common problem: anticipating a change and the growth of a successful but busy practice. You are concerned about the effect the new agents on the market will have on your workload coupled with the new referrals for non-anticoagulation patients and your staffing capacity. At this point you feel frustrated, overworked, overwhelmed, and underappreciated. Like most practitioners you have had little time to plan for future changes because you have been busy developing your practice and providing patient care. However, it is essential and wise that you develop both short-term and long-term plans to address the changes and problems that you face.
Just as you planned for the initiation of the new pharmacy service, any expansion in clinical services needs similar attention to careful planning. The good news is that now you have learned a great deal about the functions of your health care institution, the common barriers, and the factors that contribute to success. You first need to redefine your mission and vision statements to encompass a broader overall goal and guide your actions (Chapter 2, Planning and Steps to Building the Ambulatory Practice Model). Then, revisit your needs assessment. Were there other needs identified but not initially selected when you started your service? If so, gather the benchmark data again and perform a new SWOT analysis. In your daily practice, you may routinely be approached by other health care professionals to assist with drug therapy management in a particular area or with perceived pharmacotherapy needs. Lastly, during the quality improvement activities in which you have been involved, you may have identified gaps between institutional performance and goals. These are great areas in which to gather data to plan for growth. Essentially, you will need to revisit each of the steps in defining the service and building the practice and business model. This time, in developing of the model, consider how to sustain your current practice as you redefine resource needs and structure. This may also be a perfect opportunity to modify your existing services. For example, you can build in resource requests for ancillary staff or pharmacists for cross-coverage as discussed for a growing service. At this point, what are your short- and long-term solutions?
Short-Term Solutions
Ancillary Staff
In the short term, you can consider ways to maximize the use of current personnel to meet current needs. As you consider shifting your practice away from anticoagulation management, it may be possible to have the nursing staff provide point-of-care testing or vital signs for each visit as they take the vitals for each patient. This would allow you more time in another exam room where you may be conducting patient visits for hypertension or hyperlipidemia. Also, this is a good time to brainstorm to see if there are other administrative tasks with which nursing or office staff can assist. You are already using them to perform scheduling and medication refill tasks; review your daily workload; and be creative about what you can delegate.
Closing to New Referrals or Referring Back Patients
While closing to new referrals is always a difficult decision, you have to also consider that the quality of care that you provide may be impacted by a hurried clinician. As always, you need to consider what is best for the patient and your organization. A well-controlled anticoagulation patient could be managed by the physician or the nurse. Your value to patients and the organization may be in care of the more complex patient, that is, multiple medications or comorbidities. The physician and nurse may be able to handle stable patients without much added stress to their service, which would then allow you to provide the quality of care you need to give to the remainder of your patients. In essence, you could “close referrals” to a sub-set of patients and “refer back” a sub-set of patients. Trying to do it all may not be in the best interest of the patients you see or your organization. Even a 10% decrease in patient load may give you enough time to regroup. You can remain the provider’s backup for those patients who develop new problems or who become more complex.
Redistribution of Responsibilities
In the short term, you may want to brainstorm what other types of non-patient care activities occupy your time. Do you serve on any committees within the organization or provide educational in-services to staff? If so, can these responsibilities be delegated as you work to improve your practice model? When you first initiated your practice 3 years ago, you probably did not have the level of commitments that you do today. You may have to reallocate your time even though you receive professional fulfillment and growth by being involved in committees and professional organizations. By taking a step back, you will be in a better position once your practice finds its new equilibrium.
Long-Term Plan
Cross-Training Pharmacists
This is a good time to address your problem of providing coverage for vacation and professional meetings so that your patients have uninterrupted care.
CASE
You approach Dr. Busybee about cross-training another pharmacist to manage patients in your absence and help you on certain, particularly busy days. You explain under your state’s CDTM that you can assign an alternative pharmacist to work with the collaborating physician. As you look to change the scope and type of patients you care for, this may be the perfect time to integrate and cross-train a new pharmacist. Dr. Busybee agrees to this, but only if the pharmacist has the appropriate training and background (Chapter 7).
Adding Pharmacists
Another option to consider is the addition of a pharmacist as a new hire. You will need to reevaluate your resource and expense needs as it relates to your workload changes resulting from the new anticoagulation medications, medication reconciliation activities, and the increased patient referrals for medication management beyond diabetes (Chapters 2 and 3). An assessment of anticipated patient numbers for each service group and a reworked analysis (Chapter 3) will prepare you for the work-flow change that you are experiencing. The result of the reanalysis may indeed demonstrate a need for increased staffing levels. As an alternative, you can also consider a proposal to hire a temporary ambulatory care specialist until the future of the service is better defined.
Develop a Monitoring Plan
From here you should develop a plan to evaluate the service at regular intervals. This may coincide with quarterly or semiannual quality reports to streamline data collection. This will prevent any future surprises of dramatic shifts in workload and inform you so that you can anticipate needs instead of respond to changes. Establish milestones at which additional staff resources will be considered to expand services. Similarly, you will need to establish an exit plan should changes in pharmacotherapy or changes in the needs and priority of the practice occur. Use these regular time intervals to think about changes in your health system that may impact your ambulatory care practice.
Whether trying to sustain a service, grow a service, or expand into new therapeutic areas, you will find that all require careful planning and continual monitoring. The needs of your patients and the institution, changes in the environment, staffing, and finances all need to be constantly considered as you continue to build and revise your practice and business model.
Contributing to Our Knowledge
Undoubtedly, as you approached building an ambulatory care practice, you came across questions for which little information was available to guide you. Perhaps you wished that there was a published report of a successful diabetes care clinic in an institution similar to yours. You may have wished there was a better description of
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


