b. The physiologic anemia of pregnancy does not cause a reduction in oxygen delivery because of a coincident increase in cardiac output.
c. The additional intravascular fluid volume (1,000 to 1,500 mL at term) compensates for an average 300 to 500 mL blood loss with vaginal delivery and 800 to 1,000 mL estimated blood loss with cesarean section.
d. Following delivery, uterine contraction creates an autotransfusion of blood often in excess of 500 mL that also compensates for the acute blood loss from delivery.
e. In spite of mild thrombocytopenia, pregnancy is a hypercoagulable state with increases in fibrinogen and factor VII.
B. Cardiac Output
1. By the end of the first trimester, maternal cardiac output increases, on average, by 35% above prepregnancy values and continues to increase to 50% above nonpregnant values by the end of the second trimester (Fig. 45-2).

2. Labor is associated with further increases in cardiac output, which increases with each uterine contraction.
a. The largest increase in cardiac output occurs immediately after delivery, when cardiac output can be increased by 80% to 100% above prelabor values.
b. This massive increase in cardiac output represents a moment of unique risk for patients with cardiopulmonary disease, particularly those with valvular stenosis and pulmonary hypertension.
C. Systemic Vascular Resistance. In spite of increases in cardiac output and plasma volume, systemic blood pressure normally decreases secondary to a 20% reduction in systemic vascular resistance by term.
D. Aortocaval Compression
1. In the supine position, blood pressure commonly decreases as the result of aortocaval compression by the gravid uterus. Supine hypotension is manifest by symptoms of diaphoresis, nausea, vomiting, and dizziness. At term, there is almost complete occlusion of the inferior vena cava in the supine position, with return of blood from the lower extremities through the epidural, azygos, and vertebral veins.
2. Reduced sympathetic tone resulting from neuraxial or general anesthesia will impair the compensatory sympathetic nervous system response and worsen the hypotensive response to supine positioning.
3. A lateral tilt is used to avoid the hypotension that can be associated with supine positioning with neuraxial techniques for labor analgesia and operative deliveries.
E. Pulmonary Changes
1. Airway
a. During pregnancy, there is vascular engorgement with friability and edema of the mucosal lining of the oro- and nasopharynx (danger of bleeding with instrumentation of the airway and increased risk of difficult ventilation and intubation).
b. Attempts at laryngoscopy should be minimized and a smaller size cuffed endotracheal tube (6.0 to 6.5 mm internal diameter) should be considered to avoid airway edema and bleeding.
2. Minute Ventilation and Oxygenation
a. In order to accommodate the increased oxygen demand and carbon dioxide production of the growing placenta and fetus, minute ventilation is increased 45% to 50% above nonpregnant values during the first trimester and remains at this increased level for the remainder of the pregnancy.
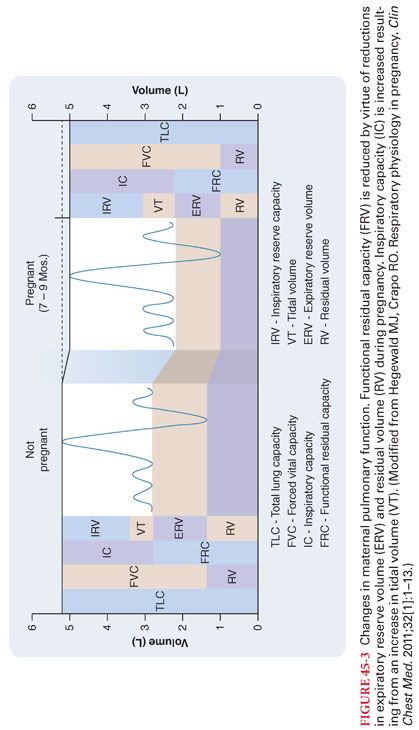
b. This greater minute ventilation is attained primarily as a result of a greater tidal volume with a small increase in the respiratory rate (Fig. 45-3).
c. Maternal Paco2 is commonly reduced from 40 mm Hg to approximately 30 mm Hg during the first trimester. Arterial oxygenation can be significantly improved by changing position from supine to lateral.
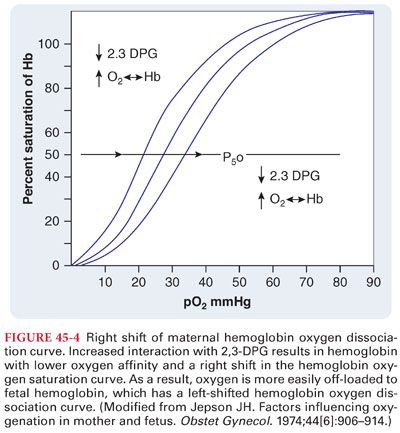
d. Maternal hemoglobin is right-shifted with the P50 increasing from 27 to approximately 30 mm Hg (Fig. 45-4). The higher P50 in the mother and lower P50 in the fetus favors off-loading of oxygen across the placenta.
3. Lung Volumes
a. During pregnancy, the growing uterus elevates the diaphragm and causes a reduction in functional residual capacity by 20% at term (see Fig. 45-3).
b. The combination of increased minute ventilation and decreased functional residual capacity results in a greater rate at which changes in the alveolar concentration of inhaled anesthetics can be achieved with spontaneous ventilation in the case of mask induction.
c. During induction of general anesthesia in a pregnant patient, desaturation occurs more rapidly than in a nonpregnant patient because of decreased functional residual capacity and increased metabolic rate. Administration of 100% oxygen prior to the induction of general anesthesia is critical to allow as much time as possible for safe airway management.
F. Gastrointestinal Changes
1. After midgestation, pregnant women are thought to be at increased risk of aspiration pneumonia with administration of general anesthesia.
a. Increased progesterone and estrogen concentrations during labor, pain, anxiety, and the administration of opioids (including those administered neuraxially) decrease gastric emptying.
b. All women in labor are considered to have full stomachs and to be at increased risk for pulmonary aspiration with induction of anesthesia.
2. Although blood flow to the liver does not change during pregnancy, markers of liver function all increase to the upper limits of normal.
3. Plasma cholinesterase (pseudocholinesterase) activity is decreased about 30% from the 10th week of gestation up to 6 weeks postpartum, but this decreased cholinesterase activity is not associated with clinically relevant prolongation of neuromuscular blockade.
G. Renal Changes. Renal blood flow and the glomerular filtration rate are increased 50% by the second trimester and remain elevated until 3 months postpartum.
H. Neurobiologic Changes
1. Pregnant patients are more sensitive to both inhaled and local anesthetic agents (minimum alveolar concentration is reduced by 30% by the first trimester of pregnancy). Unanticipated awareness is more common during cesarean section.
2. Pregnant women are more sensitive to the local anesthetics and a lower dose is able to obtain the same level of either spinal or epidural neuraxial blockade compared to nonpregnant women. At term, distention of epidural veins decreases the size of the epidural space and volume of cerebrospinal fluid (CSF) in the subarachnoid space.
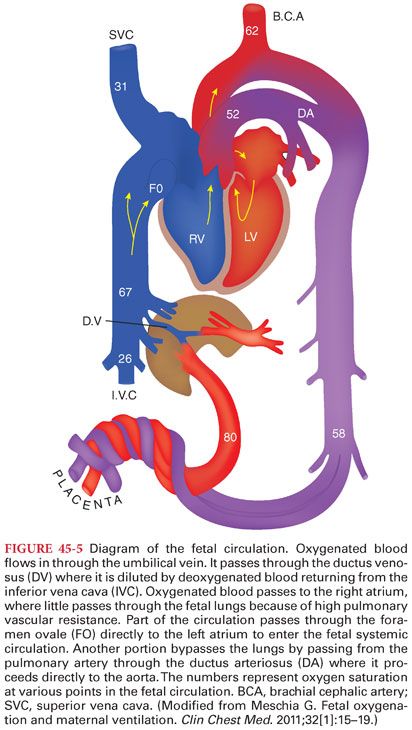
III. Uteroplacental Physiology. The placenta is composed of both maternal and fetal tissues and is the interface of maternal and fetal circulation systems (Fig. 45-5). It provides a substrate for physiologic exchange between mother and fetus without immunologic rejection.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


