Mast Cell Disease
Carlos E. Bueso-Ramos, MD, PhD
Roberto N. Miranda, MD
L. Jeffrey Medeiros, MD
Key Facts
Clinical Issues
Multiple clinical variants; common variants are
Cutaneous mastocytosis
Indolent systemic mastocytosis
Systemic mastocytosis with associated clonal hematological non-mast cell lineage disease
Aggressive systemic mastocytosis
Cutaneous mastocytosis is localized to skin
Systemic mastocytosis usually involves bone marrow
Less often: Spleen, lymph nodes, and liver ± skin
Microscopic Pathology
Lymph node
Mast cells usually present in interfollicular or diffuse pattern
Mast cells have clear/pale cytoplasm with abundant fine granules
Delicate sclerosis; eosinophils are common
Ancillary Tests
Mast cells have metachromatic granules: Giemsa(+), toluidine blue(+), chloroacetate esterase(+)
Immunophenotype: Tryptase(+), CD117/KIT(+), aberrant CD2(-/+), CD25(+/-)
± activating KIT point mutation D816V
Top Differential Diagnoses
Mast cell hyperplasia
Acute myeloid leukemia with tryptase(+) blasts
Myeloid and lymphoid neoplasms with PDGFRA rearrangements
Nodal marginal zone B-cell lymphoma
 Mast cell disease involving skin. Note macular or maculopapular brown skin lesions. The pigmentation is usually caused by an intraepidermal accumulation of melanin. |
TERMINOLOGY
Abbreviations
Systemic mast cell disease (SMCD)
Synonyms
Systemic mastocytosis (SM)
Definitions
Neoplastic proliferation of mast cells (MC), usually involving cutaneous and extracutaneous sites
SMCD is often divided into clinicopathologic subtypes
Cutaneous mastocytosis (CM): Skin is sole site of disease
Systemic mastocytosis (SM): Involvement of at least 1 extracutaneous site
± skin disease
CLINICAL ISSUES
Epidemiology
Age
Wide range; mean is 60 years
CM occurs mainly in children
˜ 50% of affected children are < 6 months of age
Gender
Slight male predominance
Site
SM usually involves bone marrow (BM), spleen
Less frequently lymph node, liver, ± skin
CM is disease confined to skin
Presentation
Indolent to aggressive disease ± multiorgan involvement
Skin manifestations
CM refers to disease restricted to cutaneous sites
Urticaria pigmentosa (UP)/maculopapular CM
Macules or macules and papules with melanin pigmentation
Lesions may urticate when stroked (Darier sign)
Affects mainly children
Usually associated with pruritus, urticaria, and dermographism
˜ 10% of patients with UP have SM; indolent > aggressive SM
Lesions in adults tend to appear as disseminated macules and papules
Diffuse CM
Diffuse thickening of skin
Almost exclusively in children
Solitary mastocytoma of skin
Single lesion without predilection for presenting site; mostly in infants
Constitutional symptoms
Fatigue, fever, weight loss
Musculoskeletal manifestations
Bone pain ± pathologic fractures
Arthralgias, myalgias
Mediator-related systemic events
Flushing, syncope, headache, anaphylaxis
Abdominal pain, diarrhea, nausea, and vomiting
Hypotension, tachycardia, respiratory symptoms
Splenomegaly more frequent than hepatomegaly or lymphadenopathy
Laboratory Tests
Serum tryptase persistently > 20 ng/mL is a minor diagnostic criterion
Hematologic manifestations
Anemia; hemoglobin (Hb) < 10 g/dL is a “C” finding
± leukocytosis, eosinophilia, monocytosis
± leukopenia; absolute neutrophil count (ANC) < 1.0 x 109/L is a “C” finding
Thrombocytosis or thrombocytopenia; platelet count < 100 x 109/L is a “C” finding
Natural History
CM is usually self-limited
Indolent SM is characterized by
Limited lesions, mild symptoms, prolonged course
Aggressive SM is characterized by
BM or multiorgan dysfunction (“C” findings)
Treatment
Osteoporosis often responds to bisphosphonates
Patients with SM usually have slowly progressive disease
Interferon-α, 2-chlorodeoxyadenosine
Patients with SM and rapidly progressive disease &/or mast cell leukemia
Polychemotherapy
Hematopoietic stem cell transplant
SM with associated clonal hematological non-mast cell lineage disease (SM-AHNMD)
Therapy mainly directed to AHNMD component
Prognosis
Excellent prognosis for patients with CM and indolent SM
Patients with aggressive SM have poor prognosis
Poor prognosis when associated with BM or organ dysfunction
Cutaneous Mastocytosis: Diagnostic Criteria
Skin lesions associated with typical clinical findings of UP
Less frequent diffuse CM or solitary mastocytoma
Typical histological infiltrates of mast cells in multifocal or diffuse pattern
Absence of features/criteria that establish diagnosis of SM
Systemic Mastocytosis: Diagnostic Criteria
Diagnosis requires 1 major criterion and 1 minor criterion, or at least 3 minor criteria
Tissue diagnosis based on examination of BM or extracutaneous organs
Major criterion
Multifocal, dense infiltrates of mast cells (≥ 15 mast cells per aggregate)
Minor criteria
> 25% of mast cells in infiltrate are spindle-shaped or have atypical morphology or
> 25% of mast cells in BM aspirate smears are immature or atypical
Detection of an activating point mutation at codon 816 of KIT (usually D816V) in BM, blood, or another extracutaneous organ
Mast cells in BM, blood, or other extracutaneous organs express CD2 &/or CD25
Serum total tryptase persistently exceeds 20 ng/mL
Except when there is associated clonal myeloid neoplasm
Criteria for Variants of Systemic Mastocytosis
All variants meet criteria for SM; in addition, distinctive features and subgroups are described
Extracutaneous mastocytoma
Unifocal mast cell tumor with low-grade cytology and without destructive growth pattern
No evidence of SM; no skin lesions
Indolent SM
No “C” findings; no evidence of SM-AHNMD
Subtype: BM mastocytosis
Absence of skin lesions
Subtype: Smoldering SM
≥ 2 “B” findings and no “C” findings
SM with associated clonal hematological non-mast cell lineage disease (SM-AHNMD)
Meets criteria for AHNMD, which include
Myelodysplastic syndrome, myeloproliferative neoplasm, acute myeloid leukemia, lymphomas, or other hematological neoplasm
Associated neoplasm meets criteria for distinct entity as defined in WHO classification
Poor prognosis
Aggressive SM
1 or more “C” findings; no evidence of mast cell leukemia; usually without skin lesions
Subtype: Lymphadenopathic mastocytosis with eosinophilia
Progressive lymphadenopathy with peripheral blood eosinophilia
Often with extensive bone involvement and hepatosplenomegaly; usually without skin lesions
Mast cell leukemia
BM biopsy specimen showing diffuse, compact infiltration by atypical, immature mast cells
BM aspirate smears show 20% or more mast cells
Mast cells usually account for ≥ 10% of peripheral blood white cells
Usually without skin lesions
Mast cell sarcoma
Unifocal mast cell tumor with destructive growth pattern and high-grade cytology
No evidence of SM
“B” Findings
BM biopsy specimen showing > 30% infiltration by mast cells (focal, dense aggregates) &/or serum total tryptase level > 200 ng/mL
Signs of dysplasia or myeloproliferation in non-mast cell lineage(s)
But insufficient criteria for diagnosis of clonal hematopoietic non-mast cell neoplasm (AHNMD)
Normal or only slightly abnormal blood counts
Hepatomegaly without liver dysfunction &/or
Splenomegaly without hypersplenism &/or
Lymphadenopathy on palpation or imaging
“C” Findings
BM dysfunction manifested by 1 or more cytopenias (ANC < 1.0 x 109/L, Hb < 10 g/dL, or platelet count < 100 x 109/L)
But no obvious clonal hematological non-mast cell hematopoietic disorder
Palpable hepatomegaly with impairment of liver function, ascites, &/or portal hypertension
Skeletal involvement with large osteolytic lesions &/or pathological fracture(s)
Palpable splenomegaly with hypersplenism
Malabsorption with weight loss due to mast cell infiltrates in gastrointestinal tract
IMAGE FINDINGS
Radiographic Findings
Radiograph of bone and bone mineral density assessment show
Osteosclerosis in ˜ 80% of patients
Osteoporosis in ˜ 30% of patients; mixed osteolytic and osteosclerotic lesions
Rare vertebral fracture, osteolytic lesions
No skeletal alterations in ˜ 20% of patients
CT Findings
Loss of corticomedullary differentiation in bones of axial skeleton
Thickening of cortical bone in appendicular skeleton
Can mimic myelofibrosis and osteosclerosis
Increased fluorodeoxyglucose (FDG) uptake in cortical bone by FDG-PET/CT scan
MACROSCOPIC FEATURES
General Features
Cut surface of spleen reveals micronodules and fibrous streaks
Lymph nodes are firm
MICROSCOPIC PATHOLOGY
Cytologic Features
Medium-sized round, oval, or spindled cells
Abundant pale/clear cytoplasm and indented nuclei
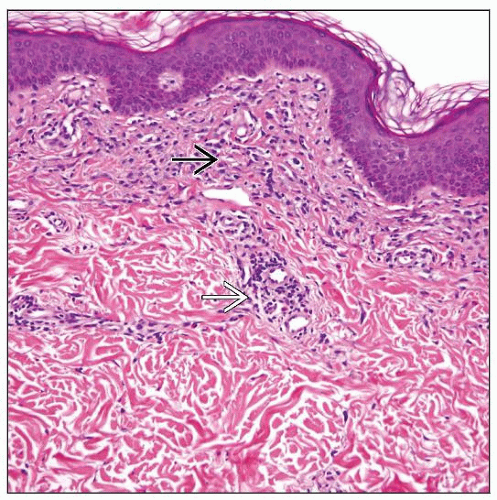
Cutaneous Mastocytosis
Spindle-shaped mast cells in papillary dermis that may extend to reticular dermis
Usually perivascular or periadnexal
Lesions in adults reveal relatively fewer mast cells than lesions in children
Diffuse CM
Sheets of mast cells filling papillary and upper reticular dermis
Solitary mastocytoma of skin
Large aggregates or sheets of mast cells that may extend into subcutaneous tissue
Mast cells with abundant granular cytoplasm
Bone Marrow
Multifocal, compact infiltrates of ≥ 15 mast cells in BM biopsy or clot specimen
Major diagnostic criterion for SM
Monomorphic, spindle-shaped mast cells that affect or stream along bone trabeculae
Mast cells appear as oval to spindle cells with faintly visible granules filling cytoplasm
Oval, round, elongated, or bilobed nuclei
Clumped chromatin with indistinct nucleoli
Predominantly paratrabecular or perivascular
Reticulin fibrosis within mast cell clusters and thickening of adjacent bone
Variable mixture of lymphocytes, eosinophils, histiocytes, and fibroblasts
Rarely, compact infiltrates composed of round, hypergranular MC
Tryptase(+) round cell infiltration of BM (TROCI-BM)
BM aspirate smears
Mast cells are found within fair distance from particles
≥ 20% mast cells in BM aspirate smears indicate mast cell leukemia
BM not affected by SM
Spleen
Splenomegaly in 25-40% of patients
“C” finding, if associated with hypersplenism
Clusters of mast cells with sclerosis around Malpighian follicles
Often associated with fibrosis or eosinophils
Less frequently, diffuse infiltration of parenchyma with minimal sclerosis
Liver
“C” finding, if associated with liver dysfunction
Small mast cell clusters in periportal tracts or in sinusoids
Mast cell clusters associated with fibrosis or eosinophils
Lymph Node
Eosinophils are commonly associated with mast cells; may be numerous
Mast cell infiltrate can be centered on arterioles
Mast cell infiltrate may be accompanied by
Prominent vascular proliferation
Follicular lymphoid hyperplasia
Lymphadenopathic mastocytosis with eosinophilia is rare subtype (˜ 10%)
Prominent, rapid development of lymphadenopathy with mast cell infiltrate
Peripheral blood eosinophilia
Features may be similar to cases with rearrangements of PDGFRα
Bone
Osteosclerotic or osteolytic lesions can be found
“C” finding, when large osteolytic lesions or pathologic fractures present
Irregular remodeling of bone trabeculae
Gastrointestinal Tract Mucosa
Mast cells can infiltrate mucosa; a “C” finding when associated with malabsorption and weight loss
Diffuse or multifocal mucosal lesions throughout intestines
Gastric rugal hypertrophy or flattening of folds
Histochemical Stains Helpful for Diagnosis
Naphthol AS-D chloroacetate esterase
Giemsa and toluidine blue highlight metachromatic cytoplasmic granules
ANCILLARY TESTS
Histochemistry
Wright-Giemsa stain
Reactivity: Positive
Staining pattern
Cytoplasmic
Toluidine blue
Reactivity: Positive
Staining pattern
Cytoplasmic
Immunohistochemistry
Tryptase(+), CD117/CKIT(+)
Highly sensitive for detecting mast cells
Tryptase helpful for identifying multifocal, compact infiltrates of atypical mast cells
CD25(+/-), CD2(-/+)
Aberrantly expressed by neoplastic mast cells
CD43(+), CD68(+/-), chymase(+/-)
B-cell antigens(-), CD3(-), CD5(-), CD7(-), MPO(-)
CD15(-), CD21(-), CD30(-), CD34(-)
MIB1/Ki-67 usually low
Flow Cytometry
Normal mast cells
High side scatter
CD9(+), CD32(+), CD33(+), CD45(+), CD117(+)
CD59(+), CD63(+), CD69(+), CD203c(+), CD23(+)
HLA-I cytoplasmic carboxypeptidase(+/-), cytoplasmic total tryptase(+/-)
CD2(-), CD14(-), CD15(-), CD16(-)
CD25(-), CD34(-), CD123(-)
Neoplastic mast cells
CD25(+) in 88% of cases, CD2(+) in 39% of cases
CD2 is often dim or negative compared with CD25
Stain with CD2 should be conjugated with bright fluorochrome, such as phycoerythrin
Abnormal mast cells in SM
Higher side scatter
Aberrant expression of CD25 (high), CD2, and CD123
Abnormally high reactivity for
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree