Mantle Cell Lymphoma
Roberto N. Miranda, MD
Key Facts
Etiology/Pathogenesis
CCND1-IGH/t(11;14)(q13;q32) resulting in Cyclin-D1 overexpression in most cases
Clinical Issues
MCL is nodal-based disease but extranodal sites of involvement are common
Spleen is common site
Splenectomy performed usually for cytopenias, pain, or less commonly, for diagnostic purposes
Small subset of MCL patients present with massive splenomegaly and minimal lymphadenopathy
Smaller subset of MCL patients have clinical picture that mimics B-PLL
Aggressive course and prominent splenomegaly
Marked peripheral blood lymphocytosis with many prolymphocytes
Microscopic Pathology
Enlarged white pulp nodules with coalescence
Red pulp involvement correlates with extent of MCL
Typical: MCL cell population is uniform, small to intermediate size, with irregular nuclear contours
Other morphologic variants of MCL can involve spleen
Pleomorphic, blastoid, prolymphocytoid
Ancillary Tests
Surface Ig(+), CD19(+), CD20(+)
CD22(+), FMC7(+), Bcl-2(+)
CD5(+), Cyclin-D1(+), CD23(−)
CCND1-IgH/t(11;14)(q13;q32)
Additional chromosomal aberrations are very common
TERMINOLOGY
Abbreviations
Mantle cell lymphoma (MCL)
Synonyms
Centrocytic lymphoma
Intermediately differentiated lymphocytic lymphoma
Intermediate lymphocytic lymphoma
Definitions
B-cell lymphoma characterized by CCND1-IGH/t(11;14)(q13;q32)
Most cases are composed of monomorphic small to medium-sized lymphocytes with irregular nuclear contours
ETIOLOGY/PATHOGENESIS
Pathogenesis
CCND1-IGH/t(11;14)(q13;q32) with Cyclin-D1 overexpression occurs on most cases
Dysregulated Cyclin-D1 overexpression accelerates transition from G1 to S phase of cell cycle
Overcomes suppressive effects of retinoblastoma (RB1) and p27kip1
Other mechanisms are required for lymphomagenesis
MCL is thought to arise from an antigen-naive, CD5(+) B cell (pregerminal center) in
Peripheral blood
Inner zone of mantle zone follicle
CLINICAL ISSUES
Epidemiology
Age
Median: 7th decade (range: 34-78 years)
Gender
M:F ratio = 2-3:1
Site
Most cases of MCL involve lymph nodes, but extranodal sites are often involved
Common extranodal sites
Peripheral blood, bone marrow, gastrointestinal tract
Liver, spleen, Waldeyer ring
˜ 40% of patients with MCL have splenomegaly
In some patients with MCL, splenic involvement is predominant
So-called splenomegalic form of MCL
Presentation
Splenic involvement by MCL is usually associated with splenomegaly
Can be massive
Laboratory Tests
Peripheral blood lymphocytosis in ˜ 25% of cases; occasionally > 200 × 109/L
Treatment
Surgical approaches
Splenectomy performed usually for cytopenias or local symptoms (e.g., pain)
Rarely performed to establish diagnosis
Adjuvant therapy
Rituximab (R) plus CHOP (cyclophosphamide, doxorubicin, vincristine, and prednisone)
R-plus-hyper-CVAD (fractionated cyclophosphamide, vincristine, doxorubicin, and dexamethasone)
Other aggressive chemotherapy regimens
Prognosis
IMAGE FINDINGS
Radiographic Findings
Splenomegaly can be detected by various imaging modalities
MCL is usually fluorodeoxyglucose (FDG) PET negative/low
± blastoid/pleomorphic variants
MACROSCOPIC FEATURES
General Features
Median weight: 1.6 kg (range: 0.7-3.8 kg)
Usually diffuse/miliary growth pattern
Occasionally large fleshy nodules
MICROSCOPIC PATHOLOGY
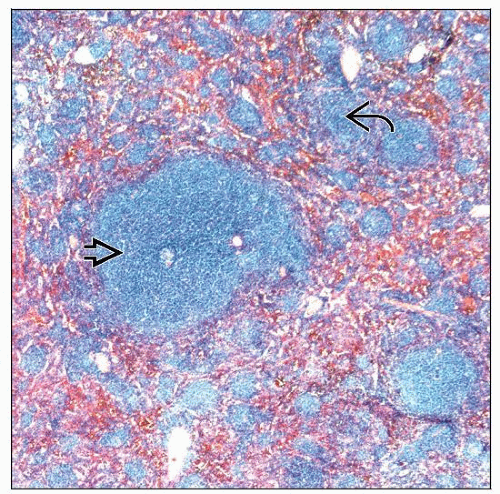
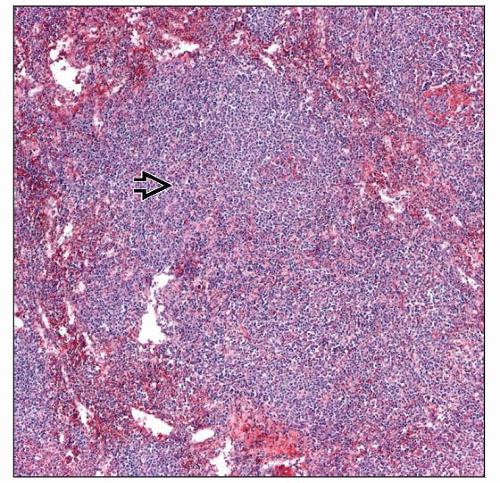
Histologic Features
Enlarged white pulp nodules with frequent coalescence
Massive white pulp expansion in some cases
± small residual germinal centers or marginal zone pattern
Red pulp involvement correlates with extent of disease
Lesser disease: Small aggregates of MCL cells in cords and sinuses
Extensive disease: Diffuse infiltration of red pulp
Scattered or clusters of histiocytes are common
Tumor cell population is uniform and typically of small to intermediate size
Round to irregular nuclear contours
Clumped chromatin and occasionally distinct nucleoli
Mitotic rate is variable
High in blastoid/pleomorphic variants
Morphologic variants of MCL
Small round: Round nuclear contours and low mitotic rate
Mimics chronic lymphocytic leukemia/small lymphocytic lymphoma
Pleomorphic: Large cells with pale cytoplasm, more prominent nucleoli, and increased mitoses
Mimics diffuse large B-cell lymphoma
Blastoid: Medium-sized cells with immature chromatin
Mimics lymphoblastic lymphoma
Prolymphocytoid: Intermediate to large cells with prominent nucleoli
More easily recognized in touch imprints than in histologic sections
Mimics prolymphocytic leukemia
Monocytoid: Small cells with abundant pale cytoplasm
Mimics marginal zone B-cell lymphoma
Examination of splenic hilar lymph nodes is helpful for diagnosis
Can assess pattern more reliably than in spleen
Diffuse, nodular, or mantle zone
Pure (> 90%) mantle zone pattern correlates with better prognosis
Cytologic features of MCL can be assessed more reliably
Environment of spleen or other extranodal sites alters cytologic features
ANCILLARY TESTS
Immunohistochemistry
Flow Cytometry
Monotypic surface Ig(+), intermediate to strong
IgM(+), IgD(+)
CD19(+), CD20(+), CD22(+), CD79a(+)
CD79b(+), FMC7(+)
CD5(+), CD10(−), Bcl-6(−)
Occasional cases are CD5(−), CD10(+), or Bcl-6(+)
More often pleomorphic/blastoid variants
CD23 usually negative but dimly positive in ˜ 10% of MCL cases
Cyclin-D1 is technically difficult to assess by flow cytometry
Cytogenetics
t(11;14)(q13;q32) is present in ˜ 70-80% of cases
Possible explanations for cases (−) by conventional cytogenetics
Poor growth of tumor cells in culture
Sampling error: e.g., only (−) BM assessed by conventional cytogenetics
Rare cases of of so-called Cyclin-D1(−) MCL
Additional nonrandom chromosomal aberrations are very common in MCL
Detected by conventional cytogenetics or comparative genomic hybridization
Gains of 3q26, 7p21, 8q24, or trisomy 12
Losses of 1p13-q31, 6q23-q27, 9p21, 11q22-q23, 13q11-q13, and 17p13-pter
Blastoid/pleomorphic variants of MCL
High frequency of additional chromosomal abnormalities
Tetraploid clones are more frequent
Higher frequency of abnormalities of 17p/P53, 9q/P16, and 8q24/MYC
Prolymphocytoid variant of MCL
High frequency of chromosome 17p/P53 abnormalities
In Situ Hybridization
FISH demonstrates the CCND1/IgH gene rearrangement in ˜ 95% of cases
Molecular Genetics
CCND1–IgH fusion gene can be shown by PCR in 30-40% of cases
Commonly used primers detect only major translocation cluster (MTC)
Southern blotting shows BCL1 locus rearrangements in 60-70% of cases
Multiple probes required for this detection rate
Additional genetic changes in MCL
Inactivating mutations of ATM gene at 11q22-23 in ˜ 50% of cases
P53 mutations, P15/16 deletions, P18 deletion
Loss of p16 and p21 expression
MYC rearrangements or amplification
Monoclonal IgH and lg Iight chain gene rearrangements
No evidence of monoclonal T-cell receptor gene rearrangements
Somatic hypermutation of Ig variable region genes uncommon (˜ 20%)
Gene Expression Profiling
Expression of ˜ 40 genes can reliably identify MCL cases
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree