Fig. 19.1
Illustration of the spread of infection from the primary anal gland abscess (a) into the surrounding tissues. (b) The commonest course is that marked X and the most rare Y (Reproduced from Parks [4], with permission from BMJ Publishing Group Ltd)
Fig. 19.2
(a–c) Illustrating the operative steps of an advancement flap (Reproduced from Hawley [26]. Reproduced by permission of Hodder Education
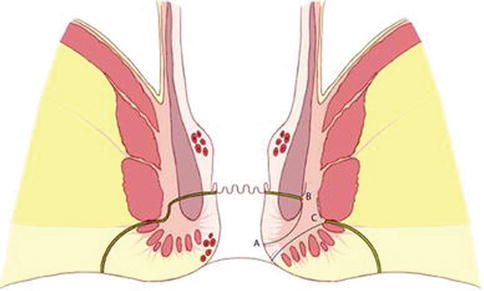
Fig. 19.3
Illustration showing the basic concept of the LIFT technique. (A) Approach via intersphincteric groove, (B) suture ligation of tract to close the internal opening and (C) suture ligation of defect in the external anal sphincter after removal of all infected granulation tissue (Reproduced from Rojanasakul [23], with permission from Springer)
References
1.
Lunniss PJ, Phillips RKS. Anal fistula: evaluation and management. In: Phillips RKS, editor. Colorectal surgery. 4th ed. Edinburgh: Elsevier Saunders; 2009. p. 223–43.
2.
The NHS Information Centre, Hospital Episode Statistics for England. Inpatient statistics, 2009–2010. www.hscic.gov.uk/hes.
3.
Sainio P. Fistula-in-ano in a defined population. Incidence and epidemiological aspects. Ann Chir Gynaecol. 1984;73(4):219–24.PubMed
5.
6.
7.
Eisenhammer S. The internal anal sphincter and the anorectal abscess. Surg Gynecol Obstet. 1956;103:501–6.PubMed
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


