Lymphomatoid Papulosis
C. Cameron Yin, MD, PhD
Key Facts
Terminology
Chronic, self-healing and recurrent erythematous papules/nodules on skin of trunk and extremities
Clinical Issues
Usually remains confined to skin
Excellent prognosis
Microscopic Pathology
4 histologic types represent a spectrum of disease
Type A is most common
Scattered large atypical Reed-Sternberg-like cells
Numerous inflammatory cells including small lymphocytes, histiocytes, granulocytes
Type B is uncommon (< 10%)
Epidermotropism and band-like dermal infiltrate
Lymphoid cells with cerebriform nuclei
Type C
Clusters or sheets of large atypical lymphoid cells with relatively few admixed inflammatory cells
Type D
Epidermotropism; CD8(+)
Ancillary Tests
Large atypical cells are CD30(+)
Small lymphocytes are T cells: Usually CD7(-)
Top Differential Diagnoses
Primary cutaneous ALCL
Systemic ALCL with cutaneous involvement
Classical Hodgkin lymphoma
Reporting Considerations
In many cases, LyP cannot be distinguished from C-ALCL without clinical information/follow-up
TERMINOLOGY
Abbreviations
Lymphomatoid papulosis (LyP)
Synonyms
Primary cutaneous CD30(+) T-cell lymphoproliferative disorder
This term also includes cutaneous anaplastic large cell lymphoma (C-ALCL)
Definitions
Chronic, self-healing and recurrent skin lesions characterized by erythematous papules/nodules on trunk and extremities
Composed of large atypical cells in marked inflammatory background
Initially described by Macaulay as “a continuing self-healing eruption, clinically benign, histologically malignant”
ETIOLOGY/PATHOGENESIS
Unknown
Suggested factors
Viral infection, reduced immunosurveillance
Chronic antigenic stimulation, direct oncogenic effect of immunosuppressive drugs
Outbreaks may be triggered by stress or illness
TNFR-associated factor-1 and cutaneous lymphocyte antigen (E-selectin ligand) are highly expressed in LyP
CLINICAL ISSUES
Epidemiology
Age
Median: 45 years (wide age range, including children)
Gender
Male to female ratio = 2-3:1
Site
Trunk and extremities most common
Genital and oral mucosa can be rarely involved
Presentation
Papular, papulonodular, or nodular skin lesions at different stages of development
Clusters or disseminated; ± ulceration
Individual skin lesions spontaneously regress within 3-12 weeks
After resolution, superficial scars can remain; hypo-or hyperpigmented
Waxing and waning clinical course; can persist for decades
LyP usually remains confined to skin
Can disseminate to regional lymph nodes
Very rarely disseminates elsewhere
Treatment
No specific therapy for most patients; follow-up with attention to skin lesion changes or development of lymphadenopathy
Therapy options include
Surgical removal ± irradiation or low-dose methotrexate for skin-restricted disease
Multiagent chemotherapy for extracutaneous lesions
Prognosis
Excellent
10-year disease-specific survival of ˜ 100%
Spontaneous regression in > 40% of patients
10-20% of patients develop a 2nd lymphoma
Mycosis fungoides (MF), C-ALCL, or classical Hodgkin lymphoma
LyP patients have increased risk for nonlymphoid cancers
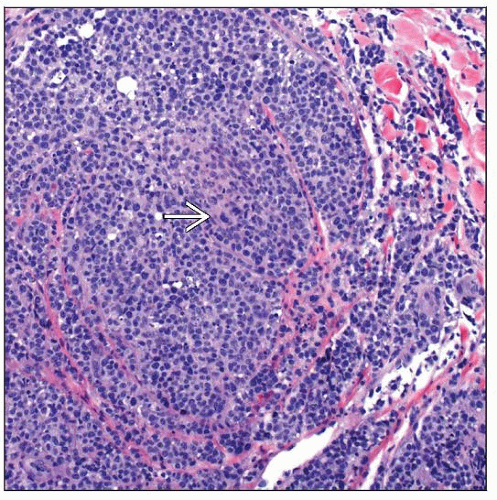
MICROSCOPIC PATHOLOGY
Histologic Features
Typically wedge-shaped lesion involving dermis
Epidermis is usually sparsely infiltrated and often ulcerated
4 histologic types have been recognized, which represent a spectrum of disease
Arbitrarily designated as A, B, C, and D
Type A is most common
Scattered large atypical Reed-Sternberg-like cells
Numerous inflammatory cells including small lymphocytes, histiocytes, neutrophils, and eosinophils
Type B is uncommon (< 10%)
Simulates MF with epidermotropism and band-like dermal infiltrate
Composed of small to medium-sized lymphoid cells with cerebriform nuclei
Cannot be distinguished from MF by histology or immunophenotyping alone
Unlike MF, type B LyP usually regresses spontaneously
Type C
Large clusters or sheets of large atypical lymphoid cells with relatively few admixed inflammatory cells
Cannot be distinguished from C-ALCL by histology or immunophenotyping alone
Type C LyP is smaller (usually < 10 mm) than C-ALCL and spontaneously regresses over time
Type D has been recently described
Characterized by marked epidermotropism and CD8(+)
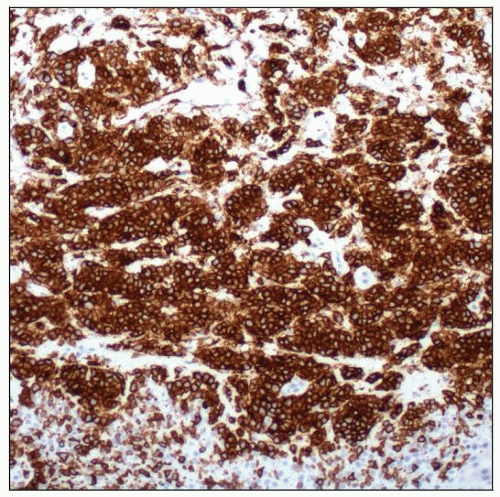
ANCILLARY TESTS
Immunohistochemistry
Types A and C
Large atypical cells are CD30(+), ALK(-)
Small lymphocytes are T cells
CD2(+), CD3(+), CD5(+), CD7 often (-); CD4(+), CD8(-)
Frequent expression of cytotoxic proteins: TIA-1, granzyme B, &/or perforin
Type B: Small cells with cerebriform nuclei are CD3(+), CD4(+), CD8(-), CD30(-)
Occasionally LyP has CD8(+) immunophenotype
More common in children
Type D: Atypical lymphocytes are CD30(+), CD3(+), CD4(-), CD8(+)