Lymphomatoid Granulomatosis
Francisco Vega, MD, PhD
Key Facts
Terminology
Extranodal angiocentric &/or angiodestructive EBV(+) B-cell lymphoproliferative disorder
Clinical Issues
Most frequent in young adults (˜ 30-40 years)
Lung is most frequent site of involvement
Number of large EBV(+) large B cells correlates with prognosis
Microscopic Pathology
Angiocentric, nodular lymphohistiocytic infiltrate
Small lymphocytes, histiocytes, plasma cells, and variable number of large lymphoid cells
Lymphocytic “vasculitis” with transmural invasion; ± necrosis; no granulocytes
Grading based on number of EBV(+) large B cells and extent of necrosis
Ancillary Tests
Large cells are B cells
CD45/LCA(+), EBER(+), CD30(+/−), CD15(−)
Smaller reactive cells are T cells: CD4 > CD8
Monoclonal IgH rearrangements
Top Differential Diagnoses
Fungal or mycobacterial infections
Necrotizing sarcoidosis
Wegener granulomatosis
Diffuse large B-cell lymphoma
Classical Hodgkin lymphoma
Peripheral T-cell lymphoma
Extranodal NK-/T-cell lymphoma, nasal type
TERMINOLOGY
Abbreviations
Lymphomatoid granulomatosis (LYG)
Synonyms
Angiocentric lymphoma
Definitions
Extranodal angiocentric &/or angiodestructive B-cell lymphoproliferative disorder composed of numerous T cells and a variable number of neoplastic EBV(+) B cells
ETIOLOGY/PATHOGENESIS
Infectious Agents
LYG presumably arises from EBV-immortalized B cells that have escaped immune surveillance
Relationship between LYG and post-transplant lymphoproliferative disorders is unclear
Clinical Associations
Congenital and acquired immunodeficiencies
Wiskott-Aldrich syndrome
HIV infection
High-dose chemotherapy
CLINICAL ISSUES
Epidemiology
Incidence
Rare
Age
Wide age range
Most frequent in young adults (˜ 30-40 years)
Gender
M:F ratio = > 2:1
Ethnicity
No clear ethnic susceptibility; more common in Western countries
Presentation
Generalized symptoms that suggest infection
Lung is most frequent site of involvement
Multiple bilateral pulmonary nodules (most frequent)
Lower lobes involved most often
Cavitation in large nodules; ˜ 25% of cases
Rare forms of lung involvement
Interstitial &/or reticulonodular patterns
Single &/or unilateral nodules
Lesions can disappear or migrate spontaneously (“wax and wane”)
Other sites of involvement
Skin (˜ 40-50%); particularly lower extremities
Central nervous system (˜ 30%)
Kidney (˜ 30%) and liver (˜ 30%)
Upper aerodigestive and gastrointestinal tracts uncommonly involved
Lymph nodes and spleen are involved rarely
Laboratory Tests
Peripheral blood
High levels of EBV DNA
Treatment
Interferon-α 2b is reported to be effective for LYG with few EBV(+) large cells (low-grade)
Aggressive chemotherapy plus rituximab for LYG with numerous EBV(+) large cells
MICROSCOPIC PATHOLOGY
Histologic Features
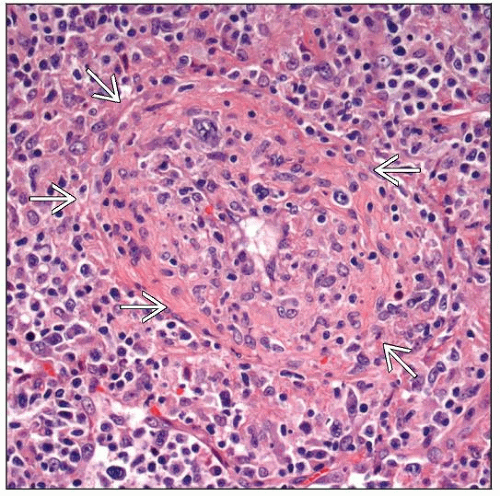
Angiocentric & angiodestructive lymphohistiocytic infiltrate
Invasion of blood vessel walls
Lymphocytic “vasculitis” with transmural invasion
Small lymphocytes admixed with histiocytes, plasma cells, and variable numbers of large atypical lymphoid cells
Granulocytes are rare or absent
Variable areas of necrosis
Vascular occlusion
Fibrinoid necrosis of blood vessels mediated by chemokines
Granulomas or multinucleated giant cells are not usually seen
Except in skin
Grading is based on number of EBV(+) large B cells and extent of necrosis
Grade 1 and 2 are considered B-cell lymphoproliferative disorder of uncertain malignant potential
Some cases may regress spontaneously or respond to interferon-α 2b therapy
Grade 3 is equivalent to diffuse large B-cell lymphoma (DLBCL)
Cytologic Features
Larger atypical cells have round to oval nuclei and prominent nucleoli
Binucleated cells are commonly seen
ANCILLARY TESTS
Immunohistochemistry
Positive for common pan-B-cell markers
CD19, CD20, CD22, CD79a, pax-5
CD45/LCA(+), CD30(+/−)
EBV-LMP1(+/−), CD15(−)
Rarely can show cytoplasmic monotypic Ig light chain in large B cells
Smaller reactive cells are T cells: CD3(+), CD4 > CD8
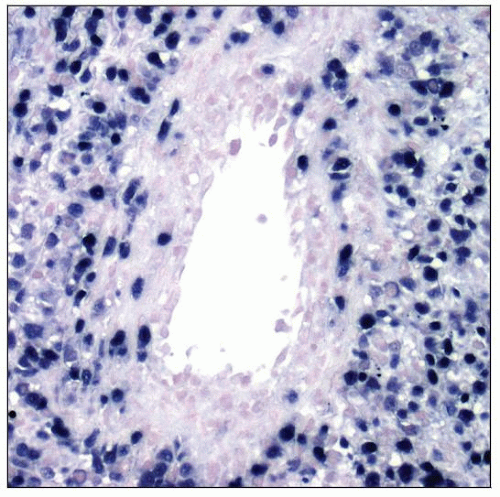
In Situ Hybridization
Large B cells are EBER(+)
Molecular Genetics
Monoclonal IgH gene rearrangements in grade 2 and 3 cases of LYG
DIFFERENTIAL DIAGNOSIS
Fungal or Mycobacterial Infections
Pulmonary histoplasmosis
Acute form
Flu symptoms, pulmonary infiltrates, and serologic evidence of Histoplasma infection
Lymphohistiocytic infiltrate with parenchymal necrosis and vasculitis (differential diagnosis with LYG grade 1)
Small necrotizing granulomas; granulocytes(+)
GMS(+), EBER(−)
Chronic form and histoplasmoma
Well-formed necrotizing granulomas; granulocytes(+)
Tuberculosis
Granulomatous inflammation with caseating necrosis; variable number of Langhans giant cells
M. tuberculosis organisms can be found in areas of necrosis
Acid-fast by Ziehl-Neelsen stain
Atypical mycobacteriosis
Immunocompromised patients &/or preexisting lung disease
Granulomatous inflammation with caseating necrosis; variable number of Langhans giant cells
Culture is required for diagnosis
Necrotizing Sarcoidosis
Adult females; frequently asymptomatic
Unilateral or bilateral lung lesions
Histologic features
Vascular granulomas surrounding, infiltrating, and destroying pulmonary arteries and veins; necrosis(+)
Wegener Granulomatosis
Systemic necrotizing vasculitis that primarily involves upper and lower respiratory tracts and kidneys
Clinical criteria
Nasal or oral inflammation
Pulmonary nodules, infiltrates, or cavities
Abnormal urinary sediment (usually microscopic hematuria)
Necrotizing granulomatous inflammation involving small arteries (by biopsy)
Limited Wegener granulomatosis
Female predominance; disease confined to lungs
Hallmark histologic features
Liquefactive &/or coagulative necrosis, geographic-shaped
Eosinophils(+); multinucleated giant cells without forming well-defined granulomas
Destructive, leukocytolytic angiitis involving arteries and veins
Diffuse Large B-cell Lymphoma
Primary DLBCL of lung represents < 1% of all lung neoplasms
Histologic features
Sheets of large neoplastic cells (centroblasts &/or immunoblasts)
± areas of coagulative necrosis
Invasion of normal pulmonary structures, such as bronchial wall and pleura, is common
Immunophenotype
B-cell antigens(+), CD10(+/−), Bcl-6(+/−), EBV(−)
DLBCL differs from grade 3 LYG in 2 ways
Grade 3 LYG resembles DLBCL but usually maintains some inflammatory background
Grade 3 LYG is EBV(+) unlike most cases of DLBCL
Primary Mediastinal Large B-cell Lymphoma (PMLBCL)
Clinical features
Enlarging mass in anterior-superior mediastinum
Frequent infiltration of local organs and structures
Histologic features
Diffuse to vaguely nodular growth pattern associated with variable sclerosis
Intermediate to large lymphoid cells
Pale cytoplasm, often result of retraction artifact
± Reed-Sternberg-like or Hodgkin-like cells
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree