Lymphocyte-rich Classical Hodgkin Lymphoma
Sa A. Wang, MD
Key Facts
Terminology
Type of CHL in which small reactive lymphocytes predominate and are associated with HRS cells
Clinical Issues
4-5% of CHL cases
Stage I or II disease; B symptoms uncommon
Peripheral lymph nodes
Survival curves of patients with LRCHL similar to patients with CHL
Early relapses followed by plateau
Unlike NLPHL patients who have late relapses without plateau
Microscopic Pathology
Nodular variant
Lymph node replaced by large, often vague nodules
Nodules are composed of expanded mantle zone small lymphocytes
Diffuse variant, uncommon
Cytologic composition is similar to that seen in nodules of nodular variant
Ancillary Tests
HRS cells have immunophenotype that supports CHL
Small lymphocytes in background have immunophenotype of mantle zone B cells
Loose FDC meshworks underlying nodules
Top Differential Diagnoses
NLPHL
Nodular sclerosis HL
T-cell/histiocyte-rich large B-cell lymphoma
Small B-cell lymphomas
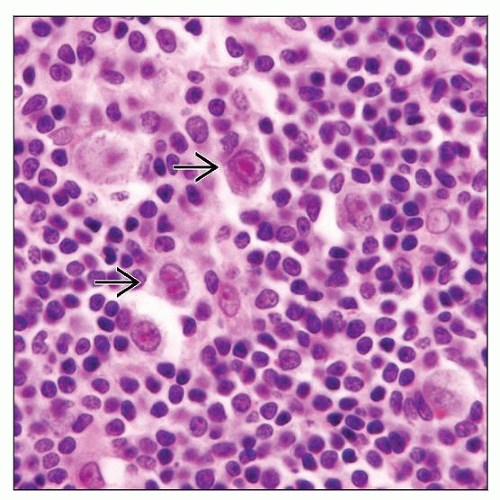
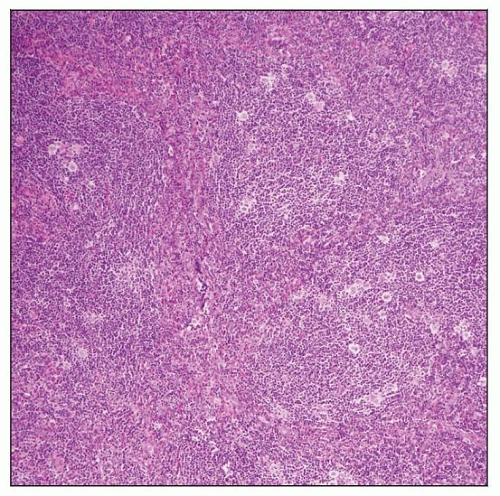 Lymphocyte-rich classical Hodgkin lymphoma (LRCHL), nodular variant, involving lymph node. The nodules are composed of many small lymphocytes and scattered Hodgkin and Reed-Sternberg (HRS) cells. |
TERMINOLOGY
Abbreviations
Lymphocyte-rich classical Hodgkin lymphoma (LRCHL)
Synonyms
Follicular Hodgkin lymphoma
Follicular Hodgkin disease
Definitions
LRCHL is type of classic Hodgkin lymphoma (CHL) in which small reactive lymphocytes associated with Hodgkin and Reed-Sternberg (HRS) cells predominate
Neutrophils and eosinophils are rare or absent in background
2 variants: Nodular and diffuse
ETIOLOGY/PATHOGENESIS
Postulated Normal Counterpart
LRCHL may be derived from B cells in outer zone of reactive germinal centers
Large cells in outer zone of reactive germinal centers have immunophenotype similar to HRS cells
CD30(+), OCT2(+), BOB1(+), Bcl-6(+/-)
Large cells surrounded by T-cell rosettes, as can occur in nodular lymphocyte predominant (NLP) HL
T cells are PD-1(+), CD57(+)
Tumorigenesis
HRS cells are derived from defective germinal center B cells with abnormal B-cell transcriptional program
HRS cells show no immunoglobulin expression
Epigenetic silencing of immunoglobulin heavy chain gene (IgH) promoters
Impaired activation of Ig promoters & enhancers
In LRCHL, B-cell transcription of HRS cells is less abnormal than in other types of CHL
Intermediate between NLPHL and CHL
NF-κB is activated in HRS cells of many cases of CHL including LRCHL
c-Rel nuclear accumulation may be responsible for malignant transformation of B cells
HRS cells regulate host response
Through expression &/or secretion of chemokines and surface ligands
Interplay of HRS cells and reactive cells determines tumor growth and local and systemic symptoms
CLINICAL ISSUES
Epidemiology
Incidence
4-5% of all cases of Hodgkin lymphoma
Age
Most common in middle-aged persons (median age: 43 years)
Gender
Male to female ratio ˜ 2:1
Presentation
Presentation of patients with LRCHL is similar to patients with NLPHL
B symptoms in ˜ 10% of patents with LRCHL
Less frequent compared with other types of CHL
Stage I or II disease in ˜ 70% of patients
Peripheral lymph node involvement is typical
Especially supradiaphragmatic lymph nodes
Mediastinal involvement is uncommon
In ˜ 15% of patients; typically not bulky
Visceral organ involvement is relatively rare
Extranodal sites include: Lungs (4%), skeleton (3%), bone marrow (2%), and liver (2%)
Although CHL is uncommon in Waldeyer ring, LRCHL is a common type in this location
Natural History
Survival curves of patients with LRCHL similar to patients with CHL
Early relapses followed by plateau
Unlike patients with NLPHL who have early and late relapses without plateau
Treatment
Drugs
Various chemotherapy regimens have been used for patients with LRCHL; most common are
Doxorubicin, bleomycin, vinblastine, and dacarbazine (ABVD) or rituximab + ABVD
Bleomycin, etoposide, doxorubicin, cyclophosphamide, vincristine, procarbazine, and prednisone (BEACOPP)
Radiation
Patients with early and intermediate-stage disease
Extended-field or involved-field radiotherapy plus chemotherapy
Radiation alone for rare early localized disease
Patients with advanced-stage disease
Local radiotherapy to debulk tumor and for residual disease, in addition to chemotherapy
Prognosis
Good to excellent with current treatment regimens
95% complete remission rate; 17% relapse rate
However, not significantly better than other types of CHL that are stage-comparable
Small subset of patients with LRCHL do poorly; fatalities due to
Relapsed/progressive disease ˜ 9%; 2nd malignancies ˜ 4%
IMAGE FINDINGS
Radiographic Findings
Peripheral lymphadenopathy
PET/CT scan useful for staging and helpful to assess therapeutic response
MICROSCOPIC PATHOLOGY
Histologic Features
Nodular variant
Lymph node is replaced by large, often vague nodules
Nodules are composed of expanded mantle zone small lymphocytes
Small, compact, often eccentric germinal centers present in subset of cases
Histiocytes are present; relatively infrequent compared with lymphocytes
Plasma cells uncommon or absent within nodules
No eosinophils or neutrophils within nodules
Loose follicular dendritic cell (FDC) meshworks underlying nodules
Highlighted by FDC markers, such as CD21, CD23, and CD35
HRS cells are scattered among small lymphocytes
Predominantly found within expanded mantle zones
Most HRS cells have classical cytologic features
Subset of HRS cells can resemble lymphocyte-predominant (LP) cells seen in NLPHL
Eosinophils and neutrophils can be present around nodules; usually infrequent
Diffuse variant
Uncommon compared with nodular variant
Diffuse replacement of lymph node architecture
Cytologic composition is similar to that seen in nodules of nodular variant
Cytologic Features
Fine needle aspiration smears show small lymphocytes and HRS cells
Diagnosis of CHL can be established
Difficult to establish specific type of LRCHL by smear examination
Possible to diagnose specific type of LRCHL if clot specimen contains tissue fragments of adequate size
ANCILLARY TESTS
Immunohistochemistry
HRS cells have immunophenotype that supports CHL
CD15(+/-), CD30(+), CD45/LCA(-)
Small lymphocytes in background have immunophenotype of mantle zone B cells
CD19(+), CD20(+), pax-5(+), IgD(+), IgM(+)
LRCHL has some features intermediate between CHL and NLPHL
Features of HRS cells closer to LP cells of NLPHL
˜ 50-60% (+) for OCT1, OCT2, and BOB1
Bright pax-5(+/-); CD20(+) in ˜ 30% of cases
Bcl-6(+) in 30% of cases
Features of HRS cells closer to typical cells of CHL
CD15(+/-), CD30(+), MUM1(+), CD45/LCA(-)
Expression of nuclear Rel, Rel-B, p-50, and TRAF1 consistent with NF-κB activation
EBV-LMP1(+) in ˜ 40% of cases; EMA usually (-)
Microenvironment of LRCHL is similar to NLPHL
Numerous small B cells in background
FDC networks in tumor nodules
T cells form rosettes around HRS cells: Often PD-1(+), CD57(+), &/or CD3(+)
Flow Cytometry
Numerous polytypic B cells
Mature T cells with normal immunophenotype
In Situ Hybridization
EBER(+) in HRS cells in ˜ 40% of cases
PCR
Monoclonal Ig gene rearrangements shown by singlecell PCR of HRS cells
DIFFERENTIAL DIAGNOSIS
Nodular Lymphocyte Predominant Hodgkin Lymphoma (NLPHL)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree