Lymphadenopathy Associated with Joint Prostheses
Roberto N. Miranda, MD
Key Facts
Terminology
Lymphadenopathy caused by abraded metal debris and cementing substances drained from sites of joint prostheses
Etiology/Pathogenesis
Hip and knee replacements are most frequent sites
Cementing materials include mainly polyethylene, which is birefringent
Clinical Issues
Pelvic lymph nodes are enlarged in patients who undergo hip replacement
Macroscopic Features
Cut surfaces of enlarged lymph nodes appear dark brown or black
Microscopic Pathology
Sinuses are markedly distended by histiocytes
Histiocytes are polygonal with abundant granular or foamy cytoplasm
Black pigment can be present
Polyethylene is transparent on routine stains; upon polarized light examination appears as birefringent
0.5-50 µm slender needles or flakes
Usually no acute inflammation or necrosis
Top Differential Diagnoses
Nonspecific sinus histiocytosis
Infectious etiologies of histiocytosis
Storage diseases
Rosai-Dorfman disease
Metastatic carcinoma to lymph nodes
TERMINOLOGY
Definitions
Lymphadenopathy caused by abraded metal debris and cementing substances drained from sites of joint prostheses
ETIOLOGY/PATHOGENESIS
Environmental Exposure
Lymphadenopathy associated with use of metal prostheses to replace large joints
Hip and knee replacements are most frequent sites
Abraded metallic debris can be found in regional or distant lymph nodes
Rarely found in bone marrow, liver, and spleen
Various materials used in construction of hip and knee replacements may be found in lymph nodes
Materials include stainless steel, cobalt, chromium, titanium, zirconium, nickel, barium, and ceramic
Most modern joint prostheses are made of stainless steel or cobalt-chrome alloy
Cementing materials include mainly polyethylene, which is birefringent
Polyethylene or ceramic are mostly used to fashion articulating surface
Titanium dioxide appears as black dusty pigment within histiocytes
Wear debris is released in periarticular tissues
When wear is excessive, local foreign body giant cell reaction occurs in joint
Tissue macrophages clear debris by draining particulate material to regional lymph nodes
CLINICAL ISSUES
Presentation
Pelvic lymph nodes are enlarged in patients who undergo hip prostheses
Incidentally found in patients undergoing genital or urinary tract staging surgery
May raise concern of malignancy
Distant sites to prosthesis may also show histiocytic reaction
Wear debris that is released into periarticular tissue elicits histiocytic reaction
Inflammatory reaction contributes to further wear of prosthesis and occasionally leads to fracture
Treatment
Lymph node removal confirms diagnosis of lymphadenopathy associated with prostheses
Excludes other causes of lymphadenopathy
No other therapy required
Prognosis
Lymphadenopathy associated with prosthesis is benign; no impact on survival
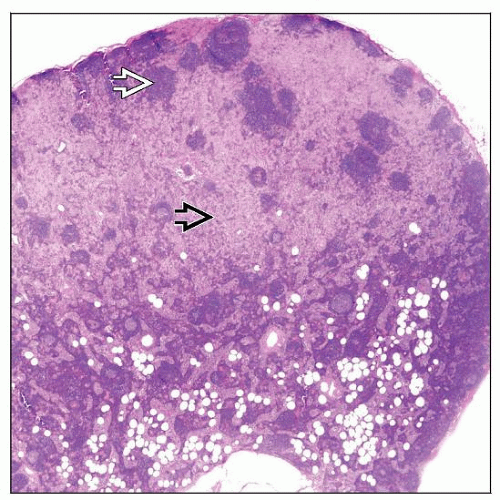
MACROSCOPIC FEATURES
General Features
Lymph nodes are usually 1-2 cm in diameter
Cut surface of lymph nodes appears dark brown or black
MICROSCOPIC PATHOLOGY
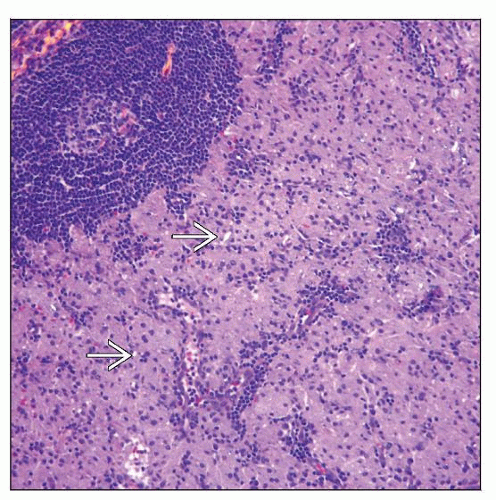
Histologic Features
Sinuses are markedly distended and occupied by polygonal histiocytes with abundant granular or foamy cytoplasm
Occasionally granulomatous reaction &/or necrosis is also present
On routinely stained H&E sections, metals appear as black nonrefringent 0.5-2 µm particles
Rarely these particles can be up to 100 µm
Polyethylene is transparent on routine stains; upon polarized light examination it is birefringent
Polarized light examination shows birefringent 0.5-50 µm slender needles or flakes
Histiocytes are PAS positive
ANCILLARY TESTS
Immunohistochemistry
Histiocytes are: Lysozyme(+), α-1-antitrypsin(+), α-1-antichymotrypsin(+), and cathepsin-D(+)
Cytokeratin(-), CD1a(-) and S100 protein(-)
Electron Microscopy
Histiocytes demonstrate abundant lysosomes
Energy dispersive x-ray elemental analysis (EDXEA) shows characteristic peaks for cobalt-chromium and titanium
DIFFERENTIAL DIAGNOSIS
Sinus Histiocytosis
Nonspecific histiocytic reaction in sinuses of lymph node
Expansion of sinuses due to histiocytes, which usually lack abundant foamy cytoplasm
Fungal Lymphadenitis
Aspergillus, Candida, and Histoplasma species most common
More common in immunosuppressed patients
Histiocytosis can be present in any lymph node compartment
Lack pigment; no polarizable material
Often associated with necrosis, acute inflammation, and foreign-body giant cells
Stains for fungi (GMS, PAS) should be performed
Cultures are valuable to identify specific organism
Mycobacterial Infections
Mycobacteria associated with histiocytosis include M. tuberculosis, M. avium, and M. leprae
Histiocytosis present in paracortical areas and sinuses
Lack pigment; no polarizable material
Epithelioid histiocytes, giant cells, granulomas, and necrosis are common
Stains for acid-fast bacilli should be performed
Cultures are valuable to identify specific organism
Storage Diseases
A number of storage diseases can cause histiocytosis in lymph nodes
Histiocytes can involve any lymph node compartment
Metastatic Carcinoma in Lymph Nodes
Metastatic carcinoma in lymph nodes can morphologically mimic histiocytosis
Lobular carcinoma of breast may mimic sinusoidal hyperplasia
Neoplastic cells can have abundant foamy cytoplasm and bland-appearing nuclei
Other primary sites of cancer in which cells can be histiocyte-like or foamy
Prostate, bladder, uterine cervix
Silicone Lymphadenopathy
Lymphadenopathy secondary to breast prosthesis shows sinus histiocytosis with fine or coarse vacuolization
Usually involves axillary lymph nodes
Rosai-Dorfman Disease
This histiocytic disorder typically begins in sinuses but can extend into other areas
Histiocytes are large with abundant cytoplasm and single central nucleus
Emperipolesis is usually present; can be obvious or more subtle
Histiocytes are strongly S100 protein(+)
Whipple Disease
Caused by bacterium Tropheryma whipplei
Patients commonly present with fever, diarrhea, and substantial weight loss
Lymph nodes in mesentery and abdomen most often affected
Histiocytes with foamy cytoplasm involving sinuses and other lymph node compartments
Histiocytes contain abundant PAS(+), diastase-resistant material
Cystic spaces, granulomatous inflammation, and epithelioid histiocytes are common
Presence of organisms can be shown by
Immunohistochemistry: Monoclonal antibody specific for T. whipplei is available
Electron microscopy: Rod-shaped bacillary body with trilaminar plasma membrane
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree