WHO 1973 classification
2004 WHO/ISUP classification
Urothelial papilloma
Urothelial papilloma
Grade 1
Papillary urothelial neoplasm of low malignant potential
Grade 2
Low grade papillary urothelial carcinoma
Grade 3

High grade papillary urothelial carcinoma
Carcinoma in situ
Carcinoma in situ
The authors of the 2004 WHO/ISUP classification clearly stated that their work was still in progress [8]. They also mentioned that, as a group of genetically stable tumors, the noninvasive LGPUCs most likely do not deserve to be designated as cancers. Noninvasive LGPUC remains an anomaly in cancer reporting. No other cancers in the human body (unless it is carcinoma in situ) are called carcinoma by a pathologist in the absence of invasion or are reported as such. Perhaps, it is time for the WHO, ISUP, and other interested groups, e.g., urologists, to address this anomalous terminology.
Definitions
Histologic Definition of Urothelial Papilloma [8]
Urothelial papilloma is defined as a discrete delicate papillary growth with a central fibrovascular core lined by urothelium indistinguishable from that of the normal urothelium (usually not more than seven cells thick).
Histologic Definition of Papillary Urothelial Neoplasm of Low Malignant Potential [8]
PUNLMP is defined as a papillary urothelial tumor that resembles urothelial papilloma with delicate papillae, but has increased cellular thickness of normal-appearing urothelium, usually more than seven cells thick. Cytologically, there is absent to minimal variation in nuclear atypia, although the nuclei might be slightly enlarged and elongated compared to normal.
Histologic Definition of Low-Grade Papillary Urothelial Carcinoma [8]
LGPUCs are usually small, confined to the urothelium without stromal invasion, and are treated by local excision [3]. They are characterized by thin papillary fronds that show frequent branching, minimal fusion, orderly appearance, and mild variations in architectural features. In contrast to urothelial papilloma or PUNLMP, there is mild but recognizable nuclear atypia such as variations in polarity, size, shape, nuclear border, and chromatin pattern.
Histologic Definition of Urothelial Dysplasia: Flat Low-Grade Intraurothelial Neoplasia [8]
Flat low-grade intraurothelial neoplasia is a flat lesion showing minimal architectural disorganization and some cytologic atypia that is not severe enough to qualify for the diagnosis of CIS. These lesions show variable and often visible loss of polarity. The nuclei of the cells may have irregular nuclear borders, slightly altered chromatin pattern, inconspicuous nucleoli, and rare mitoses.
Cytologic Definition of Low-Grade Urothelial Neoplasia
In keeping with the 2004 WHO/ISUP terminology, low-grade urothelial neopl asia (LGUN) is regarded as a combined cytologic term for low-grade papillary urothelial neoplasms (LGPUN) (which includes urothelial papilloma, PUNLMP and LGPUC) and flat, low-grade intraurothelial neoplasia. We support the view, which represents the current consensus in the field of cytopathology that we should not try to differentiate these entities in urinary tract cytologic specimens [9–11]. Most importantly, it is crucial to separate these entities from HGUC and CIS, which are discussed in Chap. 6. We also recognize that cytologic distinction between low-grade lesions and normal urothelium is extremely difficult. Therefore the only circumstances in which we can make a definitive diagnosis are described below.
Cytologic Criteria of LGUN (Regardless of the Specimen Type: Voided or Instrumented)
Three-dimensional cellular papillary –> clusters (defined as clusters of cells with nuclear overlapping, forming “papillae”) with fibrovascular cores including capillaries (Figs. 7.1, 7.2, and 7.3a). Only in the presence of this feature is the definitive cytologic diagnosis of LGUN possible [9].
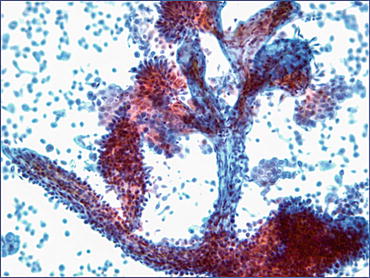
Fig. 7.1
Positive for LGUN (composite). (a) Highly cellular specimen composed of numerous tissue fragments. (b)–(d) Some fragments show three-dimensional papillary configuration. Fibrovascular cores are appreciated in the center of papillary structures (Renal pelvic washing, CS, (a)–(c) low mag. (d) medium mag.)
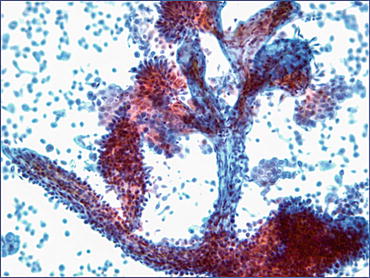
Fig. 7.2
Positive for LGUN. Three-dimensional papillary structures have central cores. Notice mild cytologic atypia and disorganization of cells forming papillae. Photo courtesy of David Wilbur (Renal pelvic washing, CS, medium mag.)
Fig. 7.3
Positive for LGUN. (a) Three-dimensional cluster of cells with nuclear overlapping, forming papillae. There is a thin capillary vessel running through the center of the cluster (Washing, TP, low mag.). (b) Positive for LGUN. Occasionally, if there is enough material left in a container, a cell block may be helpful to visualize fibrovascular cores (Washing, Cell block, H&E stain, low mag.)
In the presence of the features listed below, the cytologic diagnosis of LGUN may be considered, particularly in correlation with cystoscopic or biopsy findings [12]; however, these cases should be categorized as “Negative for High-Grade Urothelial Carcinoma (NHGUC)” (Figs. 7.4, 7.5, 7.6, and 7.7):
Fig. 7.4
Negative for HGUC with a comment suggestive of LGUN. Ill-defined three-dimensional papillary structure may represent a LGUN. No obvious capillary vessel is seen. Accumulation of red blood cells in the middle of the cluster resembles the outline of the blood vessel wall (Washing, TP, medium mag.)
Fig. 7.5
Negative for HGUC with a comment suggestive of LGUN. (a) Highly cellular specimen with numerous three-dimensional tissue fragments. No fibrovascular cores were found (Washing, TP, low mag.). (b) Negative for HGUC with a comment suggestive of LGUN. Abundant single uniform cells in a shape of “cercaria” with elongated tails and eccentrically located nuclei (Washing, TP, high mag.)
Fig. 7.6
Negative for HGUC with a comment suggestive of LGUN. A cell cluster is composed of urothelial cells with mild cytologic atypia, increased nuclear/cytoplasmic ratios, nuclear overlapping, anisocytosis, slightly irregular nuclear membranes, and dense cytoplasm (Washing, TP, high mag.)
Fig. 7.7
Negative for HGUC with a comment suggestive of LGUN. A cell cluster composed of urothelial cells with mild cytologic atypia demonstrates increased nuclear/cytoplasmic ratios, oval nuclei with occasional grooves and slightly irregular nuclear borders (Washing, TP, high mag.)
The following features, although previously reported as characteristic for LGPUC [13–15], may also be associated with high-grade urothelial carcinoma (HGUC) [16]. In the absence of other HGUC characteristics, these cytomorphologic features may suggest a LGUN lesion (see Fig. 7.4). Again, these cases should be categorized as NHGUC:
Explanatory Notes
Explanatory Note 1. Considering that the histologic definition of LGPUC includes only minimal variation in cytologic features, mainly mild nuclear enlargement and irregularity of the nuclear contours, the recognition of LGPUC separate from urothelial papilloma and PUNLMP in urine cytology is practically impossible. Relatively few studies have been done on cytopathology specimens to define the cytologic features of LGPUC in urine specimens. Although earlier reports [13, 14, 17] listed three key morphologic features based on which the diagnosis of LGPUC could be made (nuclear enlargement, slight nuclear contour irregularity, and cytoplasmic homogeneity), the reported sensitivity and interobserver agreement for cytologic diagnosis of LGPUC remained low [9, 18, 19]. Those studies were based on highly selected populations of only lower urinary tract specimens, with a very high index of suspicion, retrospective reviews of the morphologic features and long-term follow-up after the initial positive cytologic diagnosis [13, 15]. Most importantly, in some of those studies, grade-2 tumors (transitional cell carcinoma, grade 2) were included in the group of low-grade tumors. Since the introduction of the 2004 WHO/ISUP classification, there has been a significant shift in grading of urothelial neoplasms. Tumors previously classified as grade 2 are now more often categorized as high-grade [5, 6, 20].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


