Low-Grade Papillary Urothelial Carcinoma
Jesse K. McKenney, MD
Mahul B. Amin, MD
Key Facts
Terminology
Papillary urothelial neoplasm with some degree of cytoarchitectural disorder and distinct but low-grade cytologic abnormality
No high-grade cytologic features (pleomorphism, mitoses toward surface and nucleoli throughout)
Clinical Issues
Mean age is 70 years
Male predilection (M:F = 3:1)
Gross or microscopic hematuria common
Complete transurethral resection
Intravesical therapies not generally used for low-grade carcinomas
Progression and death from disease occurs in < 5% of patients
Recurrence/new occurrence is common (48-71%)
Microscopic Pathology
Cells are relatively uniform in size without significant nuclear pleomorphism or nucleomegaly
Subtle variation in nuclear size may be present
Relatively fine nuclear chromatin
Loss of cellular polarity
Random distribution of cells in urothelium
Loss of linear perpendicular orientation to basement membrane
Mitotic figures are rare and distributed randomly
Top Differential Diagnoses
Papillary urothelial neoplasm of low malignant potential (PUNLMP)
High-grade papillary urothelial carcinoma
Papillary-polypoid cystitis
Papillary nephrogenic adenoma
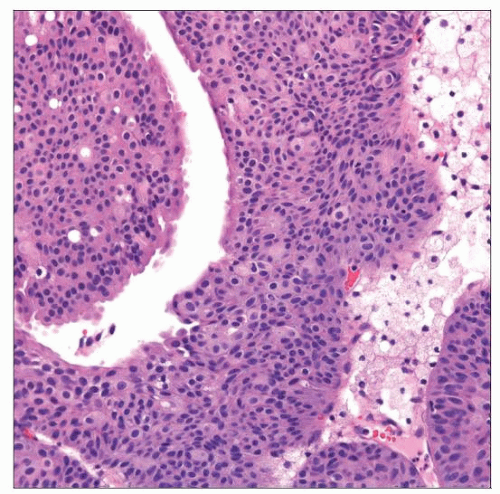
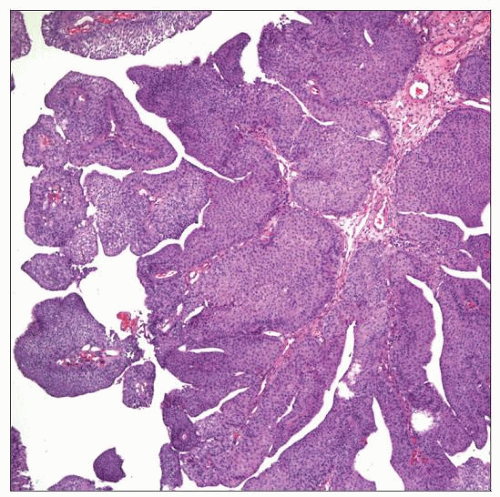 This low-grade papillary urothelial carcinoma has well-formed papillae with minimal urothelial confluence between adjacent papillae. Grading is based on the cytologic features at high magnification. |
TERMINOLOGY
Synonyms
None
Categories do not translate between nomenclature systems
Low-grade papillary urothelial carcinoma is not synonymous with WHO 1973 grade 1
Definitions
Papillary urothelial neoplasm with some degree of cytoarchitectural disorder and distinct but low-grade cytologic abnormality
No high-grade cytologic features (pleomorphism, mitoses toward surface and nucleoli throughout)
CLINICAL ISSUES
Epidemiology
Incidence
5 per 100,000 individuals per year
Age
Mean: 70 years
Gender
Male predilection (M:F = 3:1)
Site
Commonly on posterior bladder wall
Lateral wall close to ureteral orifices also common
Presentation
Gross or microscopic hematuria common
Cytology of urine may show cellular clusters/papillae suspicious for carcinoma
Treatment
Surgical approaches
Complete transurethral resection
Adjuvant therapy
Intravesical therapies not generally used for low-grade carcinomas
Prognosis
Progression and death from disease occurs in < 5% of patients
Recurrence/new occurrence is common (48-71%)
MACROSCOPIC FEATURES
General Features
Cystoscopy shows exophytic fronds of tumor
Solitary or multiple lesions
Size
Wide variation
MICROSCOPIC PATHOLOGY
Histologic Features
Cells are relatively uniform in size without significant nuclear pleomorphism or nucleomegaly
Subtle variation in nuclear size may be present
Loss of cellular polarity, random distribution of cells in urothelium
Loss of linear perpendicular orientation to basement membrane
Nuclei are often rounded with occasional irregularities of nuclear contour
Relatively fine to slightly abnormal chromatin distribution
Mitotic figures are rare and distributed randomly
Nucleoli may be present, but inconspicuous
ANCILLARY TESTS
Immunohistochemistry
Not routinely used for classifying papillary urothelial neoplasms
DIFFERENTIAL DIAGNOSIS
Papillary Urothelial Neoplasm of Low Malignant Potential (PUNLMP)
Similar to low-grade papillary urothelial carcinoma at low and intermediate magnification
Lacks distinct nuclear abnormalities
No variation in nuclear shape or size
Maintains normal perpendicular polarity to basement membrane (order)
Lack of nucleoli and mitotic figures
High-Grade Papillary Urothelial Carcinoma
Wide morphologic spectrum
High-grade features may be diffuse, focal, or patchy
Even focal high-grade features warrant a high-grade designation
Marked nucleomegaly common
Also marked variation in size and shape of nuclei
Irregular clumped nuclear chromatin
Irregular nuclear membranes
Mitotic figures may be easily identified
May be associated with invasive carcinoma
Papillary-Polypoid Cystitis
Exophytic papillary excrescences on low power
Edematous or fibrotic papillary cores
No significant branching architecture
No anastomosing epithelial growth
Broad base of excrescences may taper to slender papillae toward lumen
May have associated reactive atypia
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree