Leukemia Cutis
Jeremy C. Wallentine, MD
Key Facts
Terminology
Clinically identifiable cutaneous lesions secondary to cutaneous infiltration by neoplastic leukocytes (myeloid or lymphoid)
Clinical Issues
Presentation may precede (aleukemic LC), coincide, or manifest as recurrence of leukemia
Acute monocytic, myelomonocytic, and T-cell leukemias show the highest incidence of leukemia cutis
Occurs in 10-15% of patients with AML
Occurs in 20-70% of mature T-cell leukemias
Occurs in up to 25% of chronic lymphocytic leukemia/small lymphocytic lymphoma (CLL/SLL) cases
Microscopic Pathology
Perivascular, periadnexal, diffuse, and nodular infiltrates can be seen
Top Differential Diagnoses
Inflammatory dermatoses
Mature B-cell lymphomas
Mature T-cell lymphomas
Poorly differentiated carcinoma
Blastic plasmacytoid dendritic cell neoplasm
Diagnostic Checklist
Diagnosis requires
Careful histologic and immunohistochemical examination
Correlation with clinical data, bone marrow, and peripheral blood findings
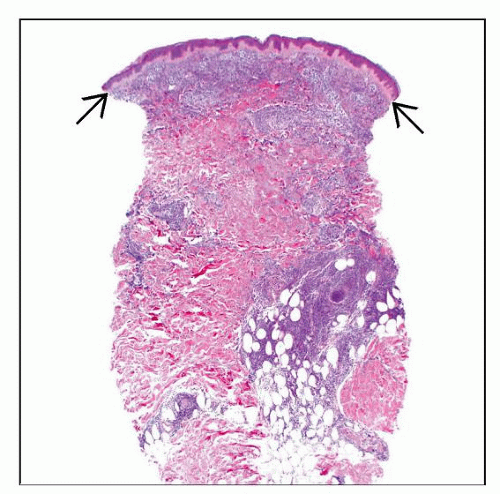
 Clinical image shows 2 small papules in a patient with acute myeloid leukemia. Histologic examination confirmed leukemic infiltrates consistent with myeloid sarcoma. (Courtesy V. Tonkovic-Capin, MD.) |
TERMINOLOGY
Abbreviations
Leukemia cutis (LC)
Synonyms
Myeloid sarcoma (MS), granulocytic sarcoma, extramedullary myeloid cell tumor, chloroma
When composed of myeloid cells
Monoblastic sarcoma
When composed of monocytic precursors
Primary extramedullary leukemia
Definitions
Clinically identifiable cutaneous lesions secondary to cutaneous infiltration by neoplastic leukocytes (myeloid or lymphoid)
Leukemia cutis commonly used to describe lymphocytic leukemias involving skin
Designated by precursor B- or T-cell lineage and chronic lymphocytic leukemia
“Myeloid sarcoma” is preferred term when leukemic cells are of myeloid or monocytic lineage
ETIOLOGY/PATHOGENESIS
Mechanisms of Skin Homing
Underlying process has not been defined
May involve coexpression of cutaneous lymphocyte antigen (CLA) and its interaction with specific chemokines
Other factors may include CCR4, TARC, and CCL22
Predilection for sites with cutaneous inflammation (e.g., Sweet syndrome, psoriasis)
CLINICAL ISSUES
Epidemiology
Incidence
Acute monocytic, myelomonocytic, and T-cell leukemias show highest incidence of leukemia cutis
LC can be observed in all forms of acute myeloid leukemia (AML)
Occurs in 10-15% of patients with AML
Varies widely with AML subtype
Up to 50% of patients with acute myelomonocytic and monocytic types
Less frequent in patients with myeloproliferative and myelodysplastic neoplasms
Rare reports of CML with LC presentation
Usually related to disease progression &/or transformation
Is seen in up to 25% of chronic lymphocytic leukemia/small lymphocytic lymphoma (CLL/SLL) cases
Occurs in 20-70% of mature T-cell leukemias
40-70% of adult T-cell leukemia/lymphoma (ATLL)
25-30% of T-cell prolymphocytic leukemia (T-PLL)
Unusual in patients with precursor B- or T-cell lymphoblastic leukemia/lymphomas (LBL) and plasma cell leukemia
Occurs in 25-30% of infants with congenital leukemia
Age
Frequency higher among children than adults
Site
Most commonly involves extremities (legs > arms)
Back, chest, scalp, and face may also be involved
Preferential involvement at sites of previous or concomitant inflammation
Sweet syndrome
Herpes zoster
Insect bites
Psoriasis
Presentation
Presentation may precede (aleukemic LC), coincide with, or manifest as recurrence of acute leukemia
Most cases present after diagnosis of systemic leukemia
< 10% present prior to blood or bone marrow involvement (aleukemic LC or primary extramedullary leukemia)
Single or multiple skin lesions
Violaceous, red-brown, or hemorrhagic papules, nodules, and plaques of varying sizes
Erythematous papules and nodules most commonly reported
Eczematous lesions
Ulcers
“Blueberry muffin” appearance
Firm blue, red, or purple nodules in generalized distribution
Term historically used to describe cutaneous involvement in children with congenital leukemia
Oral petechiae
Thickening of the gums
Oral lesions more common in adults
Rare in congenital leukemias
Other sites of extramedullary involvement are frequent (e.g., meninges)
Laboratory Tests
Lactate dehydrogenase and β2-microglobulin
Higher levels reported in patients with leukemia cutis
Serology for HTLV-1 in cases of ATLL
Treatment
Options, risks, complications
Managed by treating underlying leukemia
Systemic chemotherapy
Bone marrow transplantation
Local therapy (e.g., radiation)
Aleukemic LC should not be managed differently from patients with known leukemia
Prognosis
Poor prognosis
Generally a manifestation of disease progression
Leukemia cutis in context of congenital myelogenous leukemia is an exception
Not associated with worse prognosis
Spontaneous regression of LC without treatment has been observed
Prognosis in CLL patients is good
Exception of blastic transformation (Richter syndrome) is associated with poor prognosis
MICROSCOPIC PATHOLOGY
General Histologic Features
Low-power patterns of involvement
Perivascular &/or periadnexal
Dense and diffuse
Nodular
Subtle superficial interstitial infiltrate (rare)
Stromal fibrosis
Lineage assignment unreliable with histology alone
Myeloid and Monoblastic Sarcoma
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree