Laparoscopic Gastric Bypass
Elizabeth A. Dovec
Ronald H. Clements
DEFINITION
Obesity is a medical condition in which excess body fat has accumulated to the extent that it may have an adverse effect on health, leading to reduced life expectancy and/or increased health problems.1
The body mass index (BMI) is a measurement obtained by dividing a person’s weight in kilograms by the square of the person’s height in meters.2
BMI greater than or equal to 30 kg/m2 is obesity.
BMI greater than or equal to 35 to 39.9 kg/m2 is severe obesity.
BMI greater than or equal to 40 to 49.9 kg/m2 is morbid obesity.
BMI greater than or equal to 50 kg/m2 is super obesity.
Obesity is a leading preventable cause of death worldwide, with increasing prevalence in adults and children. Obesity is one of the most serious public health problems of the 21st century.3
The World Health Organization (WHO) predicts that overweight and obesity may soon replace more traditional public health concerns such as malnutrition and infectious diseases as the most significant cause of poor health.4 Before the 20th century, obesity was rare5; however, in 1997, the WHO formally recognized obesity as a global epidemic.6 As of 2008, the WHO estimates that at least 500 million adults (>10%) are obese.7
PATIENT HISTORY AND PHYSICAL FINDINGS
Patients should undergo comprehensive preoperative evaluation and have multidisciplinary support, with attention to psychological issues and dietary intake, for optimum outcome.
A thorough history should be performed prior to treatment, including a detailed past medical and surgical history, present medications and allergies, family history, social history, and discussions at previous attempts at weight loss.
Obesity-related comorbidities include, but are not limited to, hypertension, dyslipidemia/hyperlipidemia, diabetes mellitus, obstructive sleep apnea, chronic obstructive pulmonary disease (COPD), congestive heart failure (CHF), coronary artery disease (CAD), vascular disease, renal failure, urinary stress incontinence, polycystic ovarian syndrome (PCOS), back pain, joint pain, pseudotumor cerebri, and anxiety/depression.
SURGICAL MANAGEMENT
The goals of the surgical treatment of obesity include
Improving health
Improving quality of life
Increasing the life span
The American Society of Metabolic and Bariatric Surgery (ASMBS) and National Institutes of Health (NIH) have reached several conclusions about bariatric surgery and formulated a consensus statement. These organizations agree that bariatric surgery is the most effective treatment for morbid obesity.
Gastric bypass has been the gold standard in the treatment of the morbidly obese (BMI of ≥40 kg/m2) and severely obese (≥35 to 39.9 kg/m2) patients with obesity-associated comorbidities. It is the most frequently performed bariatric procedure in the United States.
A Roux-en-Y gastric bypass is a restrictive and malabsorptive procedure.
Preoperative Planning
Preoperative education is a vital part to the success of the patient. Patients must be instructed on what to expect both preoperatively and postoperatively.
All patients at our program undergo a surgical evaluation, medical clearances, insurance requirements, psychological evaluation, nutrition education, online information seminars, and attend a support group prior to their surgery.
A detailed bariatric diet guideline packet is provided to all patients describing each diet phase. Documented understanding of the dietary expectations is imperative.
All medications are reviewed and anticoagulation discontinuation is discussed, as applicable.
Instruction on early ambulation beginning the afternoon of surgery and continuing every 1 or 2 hours while awake thereafter
Sequential compression devices (SCDs) are on and verified to be functioning prior to the induction of anesthesia. Routine prophylactic subcutaneous anticoagulation administration is not done unless the patient has a known prior thromboembolic event or the procedure is expected to take longer than 2 hours.
Positioning
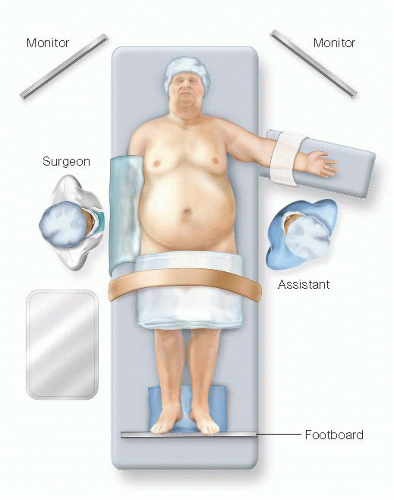
The patient is placed on the table in supine position. After satisfactory anesthesia had been administered, the patient is first secured to the bed. A thick, wide strap is placed tightly above the knees and padded well. Two pads are placed under the patient’s heels. A footboard is pushed firmly to the patient’s feet allowing the feet to turn out slightly but being cognizant not to bow the knees (FIG 1).
The left arm is left out at a 75-degree angle and secured to the arm board with a gauze wrap. If the patient’s body habitus allows, the right arm is ideally tucked at the side. The bed is positioned down as low as possible.
A standing stage is placed on the patient’s right side to be used by the operating surgeon. The assisting surgeon stands on the patient’s left side.
A 34-Fr gastric lavage tube is placed in the patient’s stomach and allowed to drain. A glove may be placed at the end of the lavage tube to prevent spillage of gastric contents. No other devices except the gastric lavage tube and endotracheal tube should be in the patient’s mouth.
TECHNIQUES
PLACEMENT OF INCISIONS
Sixteen centimeters is measured down in the left paramedian position. The skin and underlying fascia is injected with local anesthetic, and a 10-mm visual port is inserted through the left rectus sheath, identifying all layers of the abdominal wall. Pneumoperitoneum is then established. An inspection of the abdomen and pelvis is then performed ensuring there was no injury from the initial trocar placement.
The remaining five ports are then placed. The first 5-mm trocar is placed just inferior to the xiphoid process and to the left of the falciform for liver retraction. A second 5-mm trocar is placed approximately 2 cm to the right and inferior to the first 5-mm trocar placement. This 5-mm right paramedian port is also placed to the left of the falciform. A 12-mm right paramedian trocar is placed to the left of the falciform approximately one handbreadth from the second 5-mm trocar. A 5-mm left subcostal trocar is placed 2 cm below the costal margin. A final 5-mm trocar is placed 1 or 2 cm below the level of the initial port, as far lateral as possible (FIG 2).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree