Laparoscopic Gastric Band
Darren S. Tishler
Pavlos K. Papasavas
DEFINITION
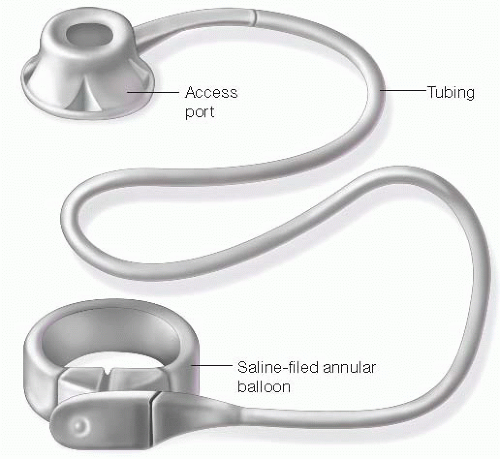
The laparoscopic adjustable gastric band (LAGB) is a Food and Drug Administration (FDA)-approved, implantable medical device for the treatment of morbid obesity and obesity-related medical comorbidities. The adjustable gastric band (AGB) consists of an adjustable saline-filled annular balloon, a segment of tubing, and a subcutaneous access port (FIG 1). This simple hydraulic system is placed around the upper portion of the stomach, just distal to the gastroesophageal (GE) junction, to create a small (approximately 30 mL) stomach pouch. The subcutaneous port is placed on the abdominal wall fascia and allows for the band stoma area to be adjusted by the addition or removal of saline solution using a noncoring needle. The AGB restricts the amount the stomach can accommodate to varying degrees, depending on the fluid volume in the band. The AGB helps to slow the progression of food from the small upper pouch to the distal stomach as well as possibly stimulating the production of gastric peptides and neuronal pathway signals related to satiety.
The AGB differs from other bariatric procedures in three main ways: It is adjustable, reversible, and involves no cutting or stapling of the stomach.
The AGB is an exclusively restrictive procedure, unlike other malabsorptive procedures such as the Roux-en-Y gastric bypass (RYGB) (see Part 2, Chapter 18) and the duodenal switch.
Patients who undergo AGB are at a low risk for developing major nutritional and vitamin deficiencies. Although medication pill size can be a factor, the AGB does not have any effect on the absorption of medications and other nutritional supplements.
PATIENT HISTORY AND PHYSICAL FINDINGS
No validated algorithm exists to prescribe the most appropriate bariatric procedure.
Although the AGB is indicated for patients with body mass index (BMI) of 30 to 40 kg/m2 with medical comorbidities or BMI greater than 40 kg/m2 with or without medical comorbidities, best results are often obtained in patients with lower BMI.
AGB typically produces best results in patients who are ambulatory and capable of performing regular aerobic activity.
In patients who fail to achieve adequate weight loss with AGB, the two most common factors are lack of exercise and depression. These issues, when present, need to be addressed both prior to surgery and during the requisite aftercare.
Ideal patients for AGB have an understanding of the importance of regular follow-up visits for band adjustments. Several studies have demonstrated an association between number of aftercare visits and weight loss. Patients require, on average, six to eight visits in the first year to achieve optimal results with the AGB procedure.1
Although patients with long-standing severe gastroesophageal reflux disease (GERD) symptoms may improve immediately after the placement of an AGB, long-term tolerance of restrictive procedures can be a problem in this subset of patients.
Allergies must be assessed, as some patients could rarely experience adverse reactions to the materials in the band.
In patients with a history of autoimmune disease, gastric banding procedures are contraindicated at this time by the FDA.2 However, several studies have demonstrated both safety and efficacy of gastric banding in this patient population.3 Contraindications to adjustable gastric banding are listed in Table 1.
Table 1: Contraindications to Adjustable Gastric Band Placement | ||||||
|---|---|---|---|---|---|---|
| ||||||
IMAGING AND OTHER DIAGNOSTIC STUDIES
Barium upper gastrointestinal (UGI) fluoroscopic evaluation is obtained in all of our patients prior to restrictive procedures to rule out the possibility of a hiatal hernia and as a screening tool for functional and structural esophageal disorders.
Routine diagnostic endoscopy is not required in all patients prior to placement of the AGB. However, it can be of use in patients with an abnormal UGI study to confirm findings of esophageal or upper gastric abnormalities or other unusual anatomy (i.e., diverticulum, paraesophageal hernia, Schatzki’s ring).
Esophageal function testing is a useful adjunct in patients with a suspected esophageal motility disorder. Patients with significant esophageal dysmotility or conditions such as achalasia and diffuse esophageal spasm should not be considered for adjustable gastric banding due to the high risk of long-term band intolerance.
SURGICAL MANAGEMENT
Preoperative Planning
LAGB should be performed at a multidisciplinary bariatric surgery program or center.
The surgeon must be comfortable with laparoscopic intracorporal suturing and procedures of the GE junction. Familiarity and preferably comfort with other bariatric surgical procedures is required.
Informed consent for the procedure should include a comprehensive discussion of alternative bariatric surgical procedures, need for long-term follow-up and adjustments, and discussion of risks (Table 2).
A preoperative very low calorie diet (VLCD) is used to deplete hepatic glycogen stores and reduce liver volume to facilitate UGI exposure. Surgery is postponed for patients with rapid weight gain just prior to the scheduled procedure.
Positioning
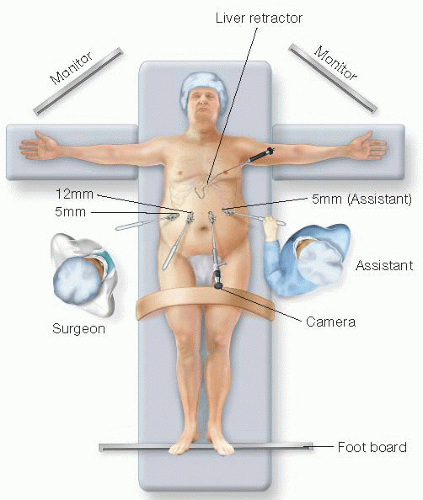
The patient is positioned supine with both arms extended. A footboard and thigh straps are used to secure the patient to the operating table.
Reverse Trendelenburg position helps to expose the upper abdomen, and steep positioning is often needed for patients with a large amount of omentum and upper abdominal fat.
The stomach is decompressed immediately after intubation with an orogastric tube. Deep muscle relaxation aids the exposure of the GE junction.
The surgeon stands to the patient’s right with an assistant to the left.
During the setup for the procedure, the scrub assistant will prepare the band per the manufacturer recommendations to flush any air from the system.
Prophylactic antibiotics are given immediately prior to incision. In addition, mechanical and pharmacologic deep vein thrombosis (DVT) prophylaxis is used.
Table 2: Risks of Adjustable Gastric Banding | ||||
|---|---|---|---|---|
|
TECHNIQUES
ENTRY TO ABDOMEN AND EXPOSURE
Laparoscopic exposure to the abdomen is obtained using an optically guided trocar in the left paramedian position approximately 3 to 5 cm below the costal margin. Either a 30-degree, 45-degree, or deflectable-tip camera is used.
Additional trocars are placed with a 12- or 15-mm trocar to accommodate the AGB insertion into the abdomen. Precise positioning of trocars ensures appropriate angle for the placement of the AGB around the upper stomach (FIG 2).
A Nathanson or similar liver retractor is placed just above the GE junction to retract the left lobe of the liver. Upward (anterior) traction on the liver retractor helps to visualize the phrenoesophageal ligament and proximal gastric anatomy. A solid and strong mounting clamp for the retractor greatly enhances the exposure. In some cases, an assistant pulling anteriorly on the retractor can facilitate exposure on a patient with both hepatomegaly and a large amount of fat around the GE junction.
DISSECTION
The hepatogastric ligament (pars flaccida) is opened using hook electrocautery or ultrasonic shears. Care must be taken to not injure a replaced or accessory hepatic artery.
The anterior GE (Belsey’s) fat pad is either lifted from the proximal stomach or removed altogether. There are often small branch vessels arising from the left gastric artery within this fat.
The angle of His (junction of greater curvature of stomach and esophagus) is minimally dissected to free the stomach from the diaphragm. This can be performed either bluntly or with hook electrocautery. Inferior traction on the fundus by the assistant facilitates this exposure (FIG 3).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree