Laparoscopic Cholecystectomy
Georgios Rossidis
DEFINITION
Laparoscopic cholecystectomy describes a procedure involving the removal of the gallbladder using a laparoscope, a fiberoptic instrument inserted into the abdomen.1
DIFFERENTIAL DIAGNOSIS
There are a number of indications for a laparoscopic cholecystectomy. The widespread use of ultrasonography has led to an increasing detection of patients with asymptomatic gallstones and the management of these patients is controversial because only 2% to 3% of these patients become symptomatic per year.
The indications in asymptomatic patients are the following:
Patients who are immunocompromised or awaiting organ allotransplantation or have sickle cell disease
Presence of gallbladder polyps that are bigger than 10 mm or are increasing in size rapidly
Porcelain gallbladder
Gallstones bigger than 3 cm in diameter in areas with high prevalence of gallbladder cancer
The indications in symptomatic patients are the following:
Episodes of biliary colic in patients with identified gallstones
Acute cholecystitis
Patients with biliary dyskinesia diagnosed with cholecystokinin-HIDA cholescintigraphy
Patients with gallstone pancreatitis with no choledocholithiasis based on imaging and laboratory values
Patients with choledocholithiasis. In most situations, cholecystectomy follows ERCP for extraction of the common bile duct stones.
PATIENT HISTORY AND PHYSICAL FINDINGS
A good medical history is necessary to provide information about associated comorbidities that may affect the patient’s tolerance to pneumoperitoneum or operative treatment in general.
Patients with cardiorespiratory disease may not tolerate the impact of CO2 pneumoperitoneum on cardiac output or CO2 elimination.
Coagulopathic disorders or anticoagulants should be identified and managed.
Medical history can identify the patients who have a higher risk for choledocholithiasis (patients with jaundice, gallstone pancreatitis, or cholangitis).
Physical examination of the abdomen reveals any surgical scars, hernias, or stomas that may alter the port placement. Previous abdominal surgery does not preclude attempt at laparoscopic cholecystectomy. Adhesive disease is a rare indication for conversion to an open procedure.
IMAGING AND OTHER DIAGNOSTIC STUDIES
Ultrasonography is now the gold standard for the noninvasive diagnosis of cholelithiasis. This imaging test is highly accurate (>96%), can be performed at the patient’s bedside, and does not require the use of ionizing radiation. Gallstones must fulfill three major sonographic criteria. They must (1) show an echogenic focus, (2) cast an acoustic shadow, and (3) seek gravitational dependence (FIG 1). Presence of a dilated common bile duct during ultrasonography is suggestive of choledocholithiasis. In the case of acute cholecystitis, ultrasound can demonstrate pericholecystic fluid, gallbladder wall thickening, and even a sonographic Murphy’s sign, documenting tenderness specifically over the gallbladder.
In atypical cases, a hepatobiliary iminodiacetic acid (HIDA) cholescintigraphy scan may be used to demonstrate obstruction of the cystic duct, which definitively diagnoses cholecystitis. Filling of the gallbladder during a HIDA scan essentially eliminates the diagnosis of cholecystitis (FIG 2).
HIDA scan is the diagnostic tool of choice in biliary dyskinesia and is performed with the concurrent administration of cholecystokinin. An ejection fraction of less than 20% is suggestive of the disease.
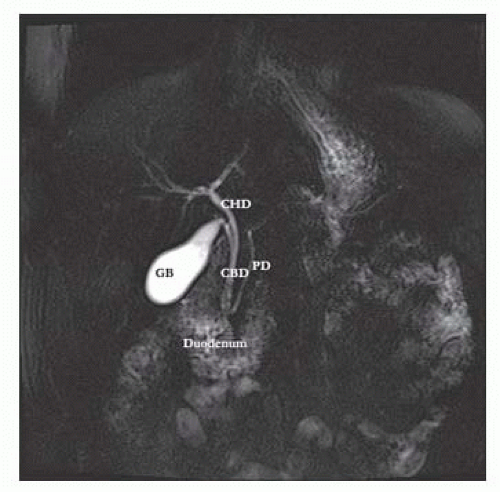
If there is suspicion of choledocholithiasis, as in patients with jaundice, pancreatitis, cholangitis, or dilated common bile duct on ultrasonography, the biliary tree can be delineated and inspected for presence of gallstones with the use of magnetic resonance cholangiopancreatography (MRCP) (FIG 3). MRCP is highly sensitive (>90%) and almost has a 100% specificity. As a noninvasive test, MRCP provides accurate imaging of the biliary tree, but in the setting of choledocholithiasis, it does not provide a therapeutic solution.
Endoscopic retrograde cholangiopancreatography (ERCP) can be used as a diagnostic and therapeutic modality (FIG 4). In the presence of stones in the common bile duct during ERCP, a sphincterotomy is performed to allow enlargement of the papilla and subsequent extraction of stones with a balloon or basket (FIGS 5 and 6). With this approach, more than 80% of all stones can be removed successfully. Larger stones may
require additional removal techniques such as mechanical or intraductal lithotripsy. ERCP has a complication rate of around 8%; complications are sedation-related, pancreatitis, bleeding, perforation, and infection.
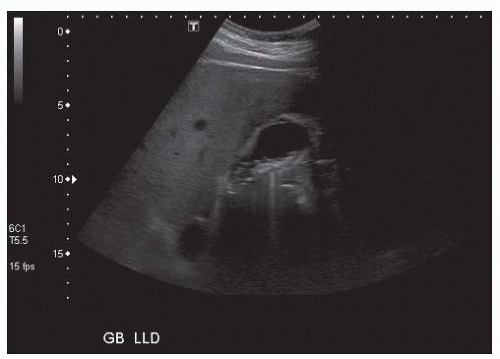
FIG 1 • Ultrasound of the abdomen showing multiple gallstones in the lumen of the gallbladder. There is no gallbladder thickening or pericholecystic fluid, thus acute cholecystitis is ruled out.
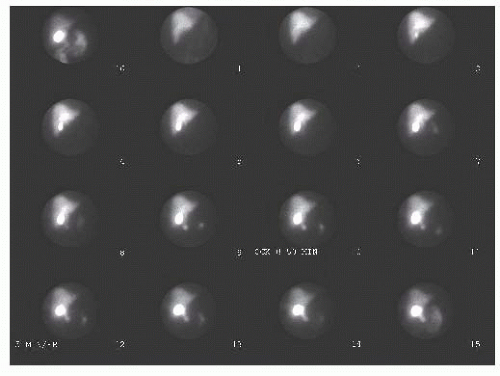
FIG 2 • HIDA cholescintigraphy scan. Filling of the gallbladder during a HIDA scan, as in this study, essentially eliminates the diagnosis of cholecystitis.
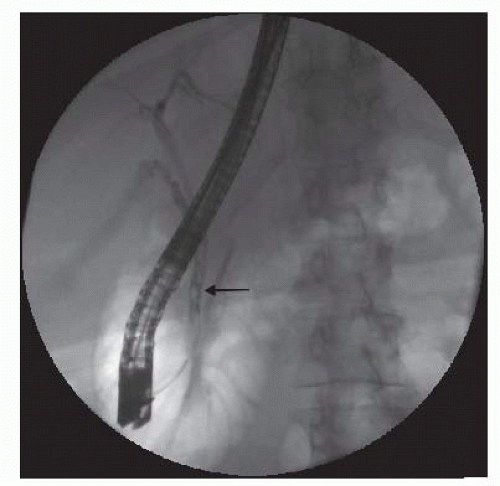
FIG 4 • Endoscopic retrograde cholangiopancreatography (ERCP). The solid arrow shows filling defect in the distal common bile duct, suggestive of choledocholithiasis.
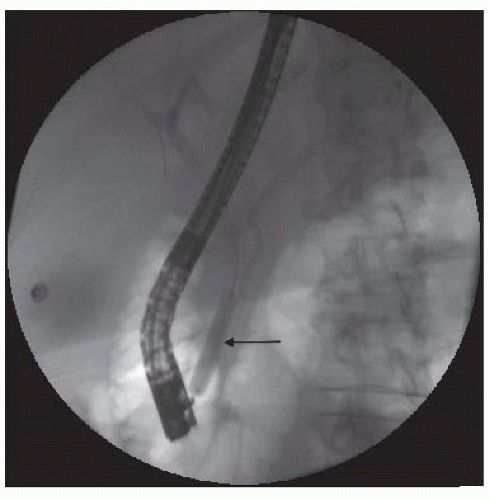
FIG 5 • ERCP on the same patient with sphincterotomy and balloon sweeping of all common bile duct stones. The solid arrow shows the endoscopic balloon.
Preoperative laboratory studies should include liver function, renal function, electrolyte, and coagulation studies. Abnormal liver function studies may reflect choledocholithiasis or primary hepatic dysfunction.
SURGICAL MANAGEMENT
Preoperative Planning
In the preoperative area, the patient is asked if any conditions exist that were not present during the last clinic visit and would factor in the operative decision making; for example, a recent myocardial infarction or other cerebrovascular event.
The patient is asked to void just prior to transfer to the operating room so as to avoid placement of a Foley catheter that is not indicated for an elective laparoscopic cholecystectomy.
The operative consent, imaging, and laboratory values are reviewed.
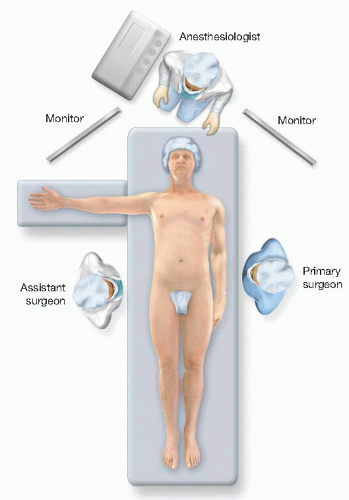
Positioning
The patient is placed in a supine position with the right arm extended and the left arm is secured along the patient’s torso (FIG 7).
A footboard is placed at the patient’s feet, and the patient is strapped at the thighs and the legs to avoid a fall from the bed during steep reverse Trendelenburg position (FIG 8).
Heel pads, sequential compression devices for deep venous thrombosis prophylaxis, and warming devices are also placed.
An orogastric tube is inserted to decompress the stomach.
The primary surgeon stands at the patient’s left and the assistant surgeon at the patient’s right (FIG 7).
Two monitors are placed at the head of the bed, one on the right and one on the left, facing the surgeon and the assistant.
The laparoscopic camera, light source, insufflation tubing, suction, and electrocautery are passed to a tower at the feet of the patient.
 FIG 8 • The patient is strapped at the thighs and legs and a footboard is placed to support the patient during reverse Trendelenburg. |
TECHNIQUES
ENTRY INTO THE PERITONEAL CAVITY AND ACHIEVING PNEUMOPERITONEUM
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree