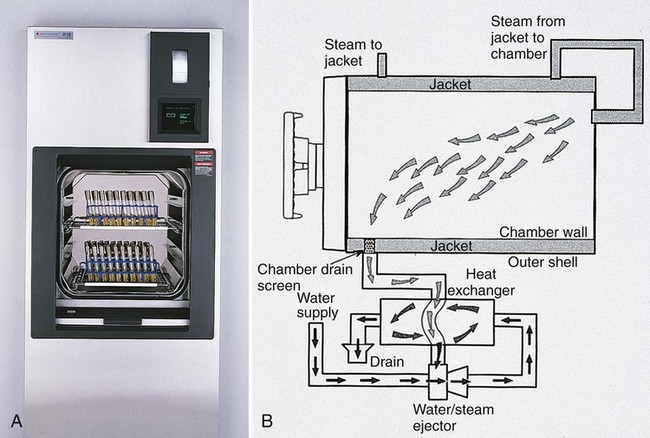
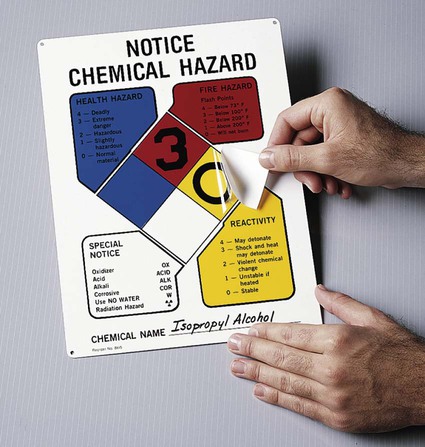
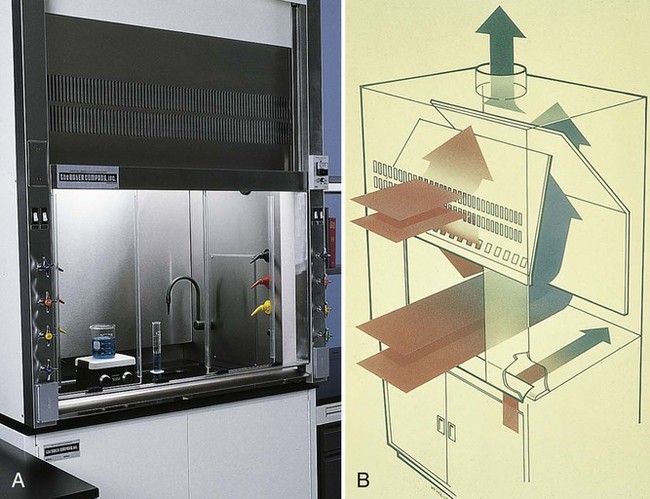
1. Define and differentiate sterilization, disinfection, and antiseptic. 2. List the factors that influence the effectiveness of disinfectants in the microbiology laboratory. 3. Describe the methods used for the disposal of hazardous waste, including physical and chemical methods, and the material and/or organisms effectively eliminated by each method. 4. Define a chemical hygiene plan and describe the purpose of the methods and items that are elements of the plan, including proper labeling of hazardous materials, training programs, and material safety data sheets. 5. Name the four types of fire extinguishers and the specific flammables that each is effective in controlling. 6. Describe the process of Universal or Standard Precautions in the microbiology laboratory, including handling of infectious materials, personal hygiene, use of personal protective equipment, handling of sharp objects, and hand-washing procedures. 7. Define Biosafety Levels 1 through 4, including the precautions required for each, and identify a representative organism for each. 8. Outline the basic guidelines for packing and shipping infectious substances. 9. Describe the management and response required during a biologic or chemical exposure incident in the laboratory. These guidelines are still incorporated into safety programs in the diagnostic microbiology laboratory. Safety programs also have been expanded to include not only the proper handling of biologic hazards encountered in processing patient specimens and handling infectious microorganisms, but also fire safety; electrical safety; the safe handling, storage, and disposal of chemicals and radioactive substances; and techniques for safely lifting or moving heavy objects. In areas of the country prone to natural disasters (e.g., earthquakes, hurricanes, snowstorms), safety programs include disaster preparedness plans that outline the steps to take in an emergency. Although all microbiologists are responsible for their own health and safety, the institution and supervising personnel are required to provide safety training to familiarize microbiologists with known hazards in the workplace and to prevent exposure. Laboratory safety is considered an integral part of overall laboratory services, and federal law in the United States mandates pre-employment safety training, followed by quarterly safety in-services. Safety training regulations are enforced by the United States Department of Labor Occupational Safety and Health Administration (OSHA). Regulations and requirements may vary based on the type of laboratory and updated regulations. It is recommended that the laboratory review these requirements as provided by OSHA (www.osha.gov). The physical methods of sterilization include: Moist heat (steam under pressure) is used to sterilize biohazardous trash and heat-stable objects; an autoclave is used for this purpose. An autoclave is essentially a large pressure cooker. Moist heat in the form of saturated steam under 1 atmosphere (15 psi [pounds per square inch]) of pressure causes the irreversible denaturation of enzymes and structural proteins. The most commonly used steam sterilizer in the microbiology laboratory is the gravity displacement type (Figure 4-1). Steam enters at the top of the sterilizing chamber; because steam is lighter than air, it displaces the air in the chamber and forces it out the bottom through the drain vent. The two common sterilization temperatures are 121°C (250°F) and 132°C (270°F). Items such as media, liquids, and instruments are usually autoclaved for 15 minutes at 121°C. Infectious medical waste, on the other hand, is often sterilized at 132°C for 30 to 60 minutes to allow penetration of the steam throughout the waste and the displacement of air trapped inside the autoclave bag. Moist heat is the fastest and simplest physical method of sterilization. The three physical methods of disinfection are: • Boiling at 100°C for 15 minutes, which kills vegetative bacteria • Pasteurizing at 63°C for 30 minutes or 72°C for 15 seconds, which kills food pathogens without damaging the nutritional value or flavor • Using nonionizing radiation such as ultraviolet (UV) light Chemical disinfectants comprise many classes, including: A number of factors influence the activity of disinfectants, including: • Temperature and pH of process • Number of organisms present (microbial load) • Concentration of disinfectant • Amount of organics present (blood, mucus, pus) • Nature of surface to be disinfected (e.g., potential for corrosion; porous or nonporous surface) In 1987, the U.S. Occupational Safety and Health Administration (OSHA) published the Hazard Communication Standard, which provides for certain institutional educational practices to ensure that all laboratory personnel have a thorough working knowledge of the hazards of the chemicals with which they work. This standard has also been called the “employee right to know.” It mandates that all hazardous chemicals in the workplace be identified and clearly marked with a National Fire Protection Association (NFPA) label stating the health risks, such as carcinogen (cause of cancer), mutagen (cause of mutations in deoxyribonucleic acid [DNA] or ribonucleic acid [RNA]), or teratogen (cause of birth defects), and the hazard class, for example, corrosive (harmful to mucous membranes, skin, eyes, or tissues), poison, flammable, or oxidizing (Figure 4-2). • Name, address, and telephone number of manufacturer • Physical and chemical properties • Health effects and first aid • Spill, leak, and disposal procedures • Personal protective equipment Fume hoods (Figure 4-3) are provided in the laboratory to prevent inhalation of toxic fumes. Fume hoods protect against chemical odor by exhausting air to the outside, but they are not HEPA-filtered to trap pathogenic microorganisms. It is important to remember that a BSC (discussed later in the chapter) is not a fume hood. Compressed gas cylinders (CO2, anaerobic gas mixture) contain pressurized gases and must be properly handled and secured. When leaking cylinders have fallen, tanks have become missiles, resulting in loss of life and destruction of property. Therefore, gas tanks should be properly chained (Figure 4-4, A) and stored in well-ventilated areas. The metal cap, which is removed when the regulator is installed, should always be in place when a gas cylinder is not in use. Cylinders should be transported chained to special dollies (Figure 4-4, B). • Rubbing the eyes or nose with contaminated hands • Inhaling aerosols produced during centrifugation, mixing with a vortex or spills of liquid cultures • Accidentally ingesting microorganisms by putting pens or fingers in the mouth • Receiving percutaneous inoculation (i.e., through puncture from an accidental needle stick) • Manipulating and/or opening bacterial cultures in liquid media or on plates, creating potentially hazardous aerosols outside of a biosafety hood Risks from a microbiology laboratory may extend to adjacent laboratories and to the families of those who work in the microbiology laboratory. For example, Blaser and Feldman1 noted that 5 of 31 individuals who contracted typhoid fever from proficiency testing specimens did not work in a microbiology laboratory. Two patients were family members of a microbiologist who had worked with S. enterica subsp. Typhi; two were students whose afternoon class was in the laboratory where the organism had been cultured that morning; and one worked in an adjacent chemistry laboratory.
Laboratory Safety
Sterilization and Disinfection
Methods of Sterilization
Methods of Disinfection
Physical Methods of Disinfection
Chemical Methods of Disinfection
Chemical Safety
Handling of Compressed Gases
Biosafety
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree