Chapter 13 Knowledge, reasoning and evidence for practice
In this chapter we examine knowledge and its place in clinical reasoning and decision making, and the relationship between knowledge and evidence for practice. The context of this paper is the current tension between three often conflicting influences on professional healthcare practice: the evidence-based practice movement, the push towards patient-centred care that incorporates patient input into clinical decision making, and management-oriented approaches to the operation of healthcare systems. We argue that one form of knowledge will not satisfy all of these demands and that understanding the nature of knowledge, its derivations and use is necessary to effectively use professional knowledge in clinical reasoning and clinical practice.
KNOWLEDGE
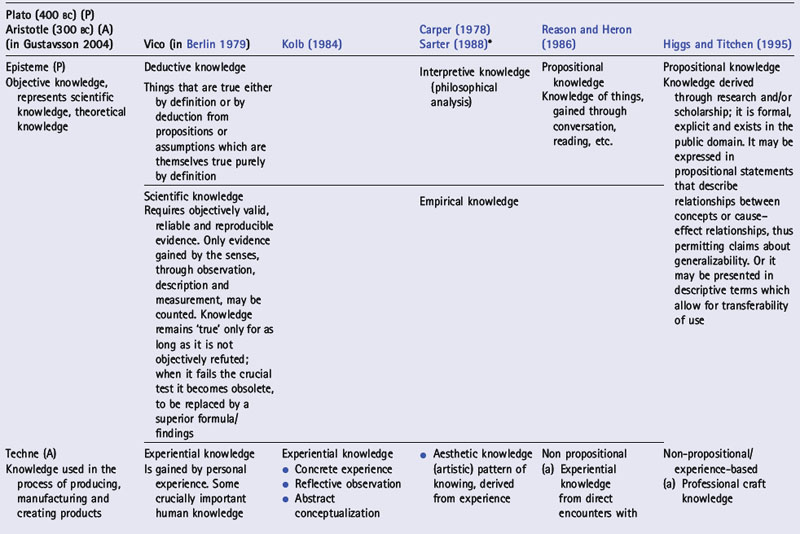
What counts as knowledge is a matter of definition. The traditional definition of knowledge as a description of the world’s structure and functions states that knowledge emerges from what we believe or hold to be true. This definition is related to the Platonic concept of episteme, from which the term epistemology derives (Gustavsson 2004). For something to be held to be true and to be accepted as a justified, true belief it must be supported by sound arguments. The concept of knowledge became much broader as a result of the contribution of Aristotle in the fourth century bc. Aristotle, in his Nicomachean Ethics (see Table 13.1), added to episteme the concepts of techne and phronesis. These three forms of knowledge deal with science, production/creativity and practical wisdom/ethics respectively, and form different ways of knowing the physical and human worlds.
Influenced by international technological and economic developments, the 1980s saw, according to Gustavsson (2004), an emerging focus on the content of practical knowledge and its relation to professional competence. Instead of the previous focus on scientific or theoretical knowledge – seen as separate from practical knowledge and as disseminated via experts and then added to practical knowledge – there was a shift to seeing such knowledge as embedded in practical actions and activities. The importance of reflection on practical experience became more clearly recognized, drawing on the philosophical perspectives of Ludwig Wittgenstein (1921), who distinguished between what can be said and that which is beyond words; he contended that we must remain silent about that which is beyond words. Other important perspectives were contributed by Michael Polanyi (1958), who presented knowledge as resting upon tacit background knowledge, and Gilbert Ryle (1949) who distinguished between knowing that and knowing how.
KNOWLEDGE CATEGORIES
The broad distinctions between ‘knowing that’ (or propositional knowledge) and ‘knowing how’ (non-propositional knowledge) (Polanyi 1958, Ryle 1949) reflect the two major categorizations of knowledge recognized in contemporary Western society. Propositional knowledge is generated formally through research and scholarship, and includes scientific knowledge (from the sciences), logic (from philosophy) and aesthetics (from the arts); it represents the ‘knowledge of the field’. Non-propositional knowledge is generated primarily through practice experience. The former is commonly regarded in modern society and in professional discourse as having a higher status, in keeping with the hegemony of the physical sciences and the scientific method. In opposing this viewpoint, Ryle (1949) argued that procedural (practical) knowledge has primacy over propositional (theoretical) knowledge, which follows rather than drives procedural knowledge. He contended that some theory is inside (part of) practice, while other (external) theory is utilized in practice. Barnett (1990) has argued that modern society is unreasonably dominated by the cognitive framework of science, with other forms of knowledge being downgraded and not even regarded as real knowledge. He argued that in a world where problems are not discrete nor solutions definite, we need knowledge beyond science.
Table 13.1 presents an overview of various ways people have categorized knowledge. Knowledge in any one category can be (and often is) translated into or subsumed within another category. For instance, knowledge derived from experience can subsequently be transformed into formal, publicly assessable propositional knowledge through theorization and/or rigorous critique and debate among practice communities. Propositional knowledge (of the field) can on the other hand also arise through basic or applied research. It can then be elaborated and particularized through practice experience to become part of the experience of the individual.
Both personally owned and publicly owned knowledge have contributions to make to professional practice. The knowledge base of an individual (Eraut 2000, p. 114) refers to ‘the cognitive resource which a person brings to a situation that enables them to think and perform … this incorporates codified (i.e. public or propositional) knowledge in its personalized form, together with procedural knowledge and process knowledge, experiential knowledge and impressions in episodic memory … [and] personal knowledge [that] may be either explicit or tacit’. Personal knowledge, an important concept in the work of Polanyi (1958), is a recurring theme through all these categorization systems. It ‘promotes wholeness and integrity in the personal encounter’ (Carper 1978, p. 20), it arises from personal and professional experiences accompanied by reflection, and it provides the individual’s frame of reference (Higgs & Titchen 1995). All forms of knowledge have limitations and must therefore be subject to continual critical reflection.
For effective clinical reasoning, we consider that health professionals rely upon the scientific knowledge of human behaviour and body responses in health and illness, the aesthetic perception of significant human experiences, a personal understanding of the uniqueness of the self and others and their interactions, and the ability to make decisions within concrete situations involving particular moral judgements. Each way of knowing, therefore, has a place in the education of health science students and in the practice of clinical reasoning.
RESEARCH KNOWLEDGE
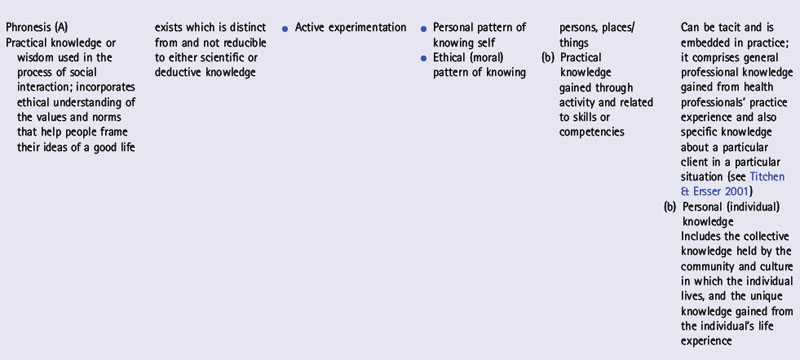
Apart from distinguishing between research- and theory-generated (propositional) knowledge and experience-based (non-propositional) knowledge, it is also useful to consider the different forms of knowledge that are generated through different research paradigms (see Table 13.2).
What can we know? What is reality?
Epistemology deals with how what exists may be known, and has been described as ‘the philosophical theory of knowledge which seeks to define it, distinguish its principal varieties, identify its sources, and establish its limits’ (Bullock & Trombley 1988, p. 279). Adopting Kuhn’s (1970) notion of paradigms means acknowledging that a paradigm is a very fundamental orientation that determines such issues as which research is relevant, which questions can be asked and addressed by research, and what constitutes and justifies evidence. Other writers take the stance that the research question determines the type of methodology and paradigm to be adopted (Domholdt 1993, Guba & Lincoln 1994). However, Kuhn would argue that it is not possible to step out of paradigms at will because they do not suit one’s questions or interests.
Table 13.2 presents three broad research paradigms and the types of knowledge associated with these paradigms.
A) THE EMPIRICO-ANALYTICAL PARADIGM
This paradigm, which underlies the medical model, has dominated the philosophy of science from the 1920s to the 1960s (Manley 1991). The scientific paradigm or empiricist model of knowledge creation utilizes the scientific method and relies on observation and experiment in the empirical world, resulting in generalizations about the content and events of the world which can be used to predict future experience (Moore 1982). In many of the health professions it is questioned whether the medical model is a sufficient, or indeed the preferred, model for the health sciences. The medical model is increasingly regarded as inadequate for addressing the breadth of human challenges faced in health care. In some situations (e.g. care of older people or people with chronic conditions, community health, industrial and occupational health) other healthcare models (e.g. biopsychosocial, person-centred, relationship-centred or emancipatory models) are seen as preferable. Such preferences have been identified by some writers in nursing (Holmes 1990, McCormack 2001), physiotherapy (Parry 1997, Shepard 1987), medicine (Borrell-Carrió et al 2004) and occupational therapy (Denshire 2004, Mattingly 1991). Practitioners in these fields identify a dissonance between the philosophical bases for practice and research (Holmes 1990, Manley 1991). There is a greater emphasis, in nursing and occupational therapy in particular, on the humanistic movement and on knowledge generated within the interpretive and critical paradigms, while at the same time research conducted in the empirico-analytical paradigm is valued for the different purposes of answering questions about efficacy and effectiveness.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree