Inverted Papilloma
Jesse K. McKenney, MD
Key Facts
Terminology
Benign urothelial neoplasm with predominantly endophytic growth pattern
Clinical Issues
Very uncommon urothelial lesion (1% of urothelial neoplasms)
Most common in trigone and bladder neck region
Recurrence rate: < 1%
Microscopic Pathology
Surface urothelium is normal
Urothelium invaginates into lamina propria
Forms thin interconnecting cords/trabeculae
Periphery of cords typically show palisading of basal cells
Central areas of cords may be spindled
Lesion has smooth pushing contour
Epithelial nests may become centrally cystic with cuboidal epithelial lining
Rare tumors have mixed inverted and exophytic patterns of urothelial papilloma
Scattered cells with “degenerative” atypia may be seen
Rare cases may contain foamy or vacuolated cytoplasm
Top Differential Diagnoses
Urothelial carcinoma with endophytic growth pattern
Nested urothelial carcinoma
Paraganglioma
Florid von Brunn nests/cystitis cystica
Carcinoid tumor
TERMINOLOGY
Definitions
Benign urothelial neoplasm with predominantly endophytic growth pattern
Involves lamina propria
CLINICAL ISSUES
Epidemiology
Incidence
Very uncommon urothelial lesion (1% of urothelial neoplasms)
Age
1st to 8th decade
Gender
Male predominance
Site
Occurs anywhere along urothelial tract
Most common in trigone and bladder neck region
Presentation
Gross or microscopic hematuria
Endoscopic Findings
Smooth or nodular polypoid structures
May be sessile or contain short stalk
Treatment
Surgical approaches
Complete transurethral resection
Prognosis
Recurrence rate: < 1%
MACROSCOPIC FEATURES
General Features
Polypoid with smooth mucosal surface
Size
Most are < 3 cm
Rare tumors may be up to 8 cm or more
Larger tumors require extensive or complete sampling
MICROSCOPIC PATHOLOGY
Histologic Features
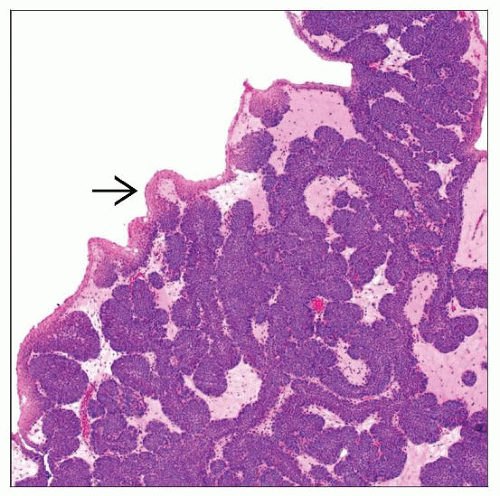
Urothelium invaginates into lamina propria
Forms thin interconnecting cords/trabeculae
Surface epithelium is normal
Presence of more than occasional exophytic papillae argues for mixed inverted and exophytic patterns of urothelial papilloma
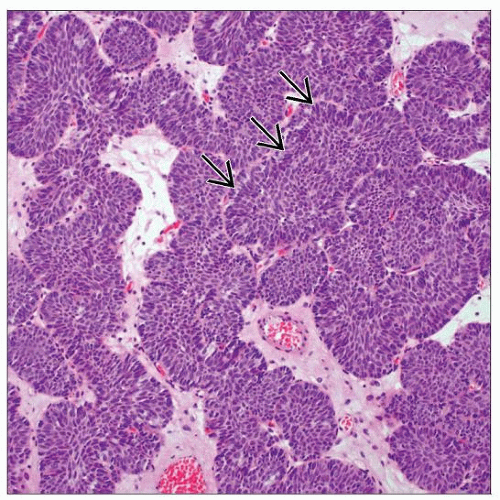
Periphery of cords typically show palisading of basal cell nuclei
Mitotic figures are rarely seen at basal layer
Central areas of cords may show cellular spindling
Lesion has smooth pushing contours
Distinct from irregular nests of invasive carcinoma
No stromal reaction
Epithelial nests may become centrally cystic with cuboidal epithelial lining
Cystitis cystica or cystitis glandularis-like patterns
Bland cytologic features
Scattered cells with “degenerative” atypia may be seen
Rare cases may contain foamy or vacuolated cytoplasm
Nonkeratinizing squamous metaplasia may be present
Predominant Pattern/Injury Type
Inverted trabeculae/cord
Predominant Cell/Compartment Type
Epithelial, urothelial
DIFFERENTIAL DIAGNOSIS
Other Urothelial Neoplasms with Endophytic Growth Pattern
Same spectrum of tumors as papillary urothelial neoplasia
Papillary urothelial neoplasm of low malignant potential, low- to high-grade carcinoma
Subtype based on thickness and cytology of neoplastic cells
Distinction has therapeutic significance
Endophytic component has expansion of trabeculae
Most useful feature on low-power examination
Surface lining shows true papillae in some cases
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree