Invasive Adenocarcinoma
Jesse K. McKenney, MD
Mahesha Vankalakunti, MD
Key Facts
Etiology/Pathogenesis
Predisposing factors
Associated with bladder exstrophy
Nonfunctioning bladder
Clinical Issues
Rare primary bladder neoplasm (< 2% of bladder malignancies)
Peak incidence in 6th decade
Most common presentation is hematuria
Poor prognosis (5-year survival rate varies from 18-47%) secondary to high stage at presentation
Microscopic Pathology
Pure glandular differentiation
Associated adenocarcinoma in situ may be seen
Ancillary Tests
CK20 positive, CK7 negative
May express villin and CDX-2
Does not express nuclear β-catenin
PAP reactivity is reported, but PSA is typically negative
Top Differential Diagnoses
Direct invasion by prostatic adenocarcinoma
Direct invasion or metastatic colorectal adenocarcinoma
Metastatic adenocarcinoma
Cystitis glandularis
Invasive urothelial carcinoma with glandular differentiation or small tubules
Müllerianosis
Urachal adenocarcinoma
 Primary adenocarcinoma is a gland-forming carcinoma with no associated component of urothelial carcinoma. Metastatic carcinoma is always a consideration when dealing with these tumors. |
TERMINOLOGY
Definitions
Primary gland-forming carcinoma of urinary bladder not associated with urothelial or squamous carcinoma component
ETIOLOGY/PATHOGENESIS
Developmental Anomaly
Associated with bladder exstrophy (~ 4-7% risk)
Chronic Irritation
Nonfunctioning bladder
May occur within urachal remnant or cyst
Obstruction
Schistosomiasis
CLINICAL ISSUES
Epidemiology
Incidence
Rare primary bladder neoplasm (< 2% of bladder malignancies)
Age
Peak incidence in 6th decade
Gender
M:F = 2.6:1
Site
Bladder base is most common
Presentation
Hematuria most common
Dysuria
Rarely mucusuria
Treatment
Radical cystectomy
Adjuvant radiation &/or chemotherapy may be employed
Prognosis
Poor prognosis (5-year survival rate varies from 18-47%) secondary to high stage at presentation
MACROSCOPIC FEATURES
General Features
Exophytic, papillary, sessile, or infiltrating mass
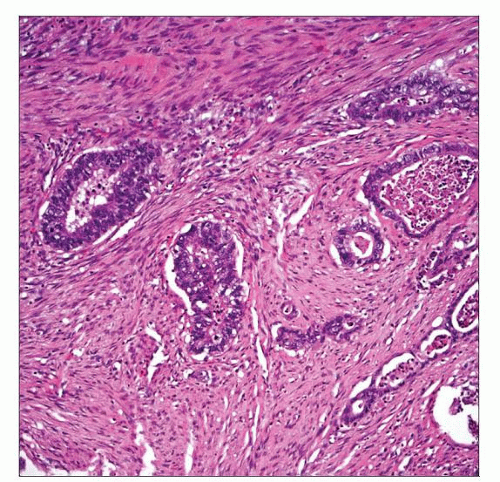
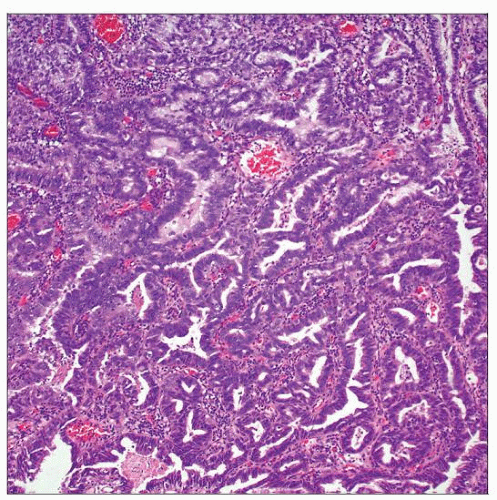
MICROSCOPIC PATHOLOGY
Histologic Features
Pure glandular differentiation
Varying patterns are described
Enteric
Adenocarcinoma, not otherwise specified
Mucinous/colloid
Signet ring cell
Hepatoid
Mixed
Not uncommonly associated with intestinal metaplasia
Associated adenocarcinoma in situ may be seen
ANCILLARY TESTS
Immunohistochemistry
Enteric adenocarcinoma may have significant overlap with colonic adenocarcinoma
CK20 typically positive
CK7 phenotype is variable, usually negative
May express villin and CDX-2
Does not express nuclear β-catenin
PAP reactivity is reported, but PSA is typically negative
Uroplakin-3 negative
DIFFERENTIAL DIAGNOSIS
Direct Invasion by Prostatic Adenocarcinoma
More common than primary adenocarcinoma
Monomorphic round nuclei with prominent nucleoli suggest prostate origin
Ductal adenocarcinoma of prostate has significant morphologic overlap
Often expresses PSA and PAP
Primary bladder adenocarcinoma may express PAP
PSMA and P501S may also be expressed by bladder adenocarcinoma
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree