CHAPTER 5 INTRODUCTION TO FOOD AS MEDICINE
Let food be your medicine and medicine be your food. (Hippocrates)
The maxim coined by Hippocrates, the father of Western medicine, around the 5th century BC, is as true today as it was then. Hippocrates observed that certain foods had the potential to both prevent and treat disease, and recognised the effects of nutritional deficiencies and excesses on health (Jensen 1993). Hippocrates’ axiom went largely ignored in the evolution of Western medicine, but the pioneering work of researchers such as Linus Pauling and Victor Rocine in the early 20th century created a renewed interest in the therapeutic value of food and its influence, both positive and negative, on health.
Together with an increasing understanding of the potential benefits and negative consequences of food choices comes an unprecedented availability of different foods. Yet despite this, a problem of oversupply has arisen in developed countries and many Australians are consuming vast amounts of kilojoule-laden, yet nutrient-deficient, foods resulting in nutritional depletion and suboptimal nutrition. Largely as a result of this phenomenon, nutrition research has shifted from focusing exclusively on deficiency states to investigating the association between disease prevention, healthy ageing and adequate dietary intake in order to optimise quality of life and long-term health (Kennedy 2006).
FUNCTIONAL FOODS
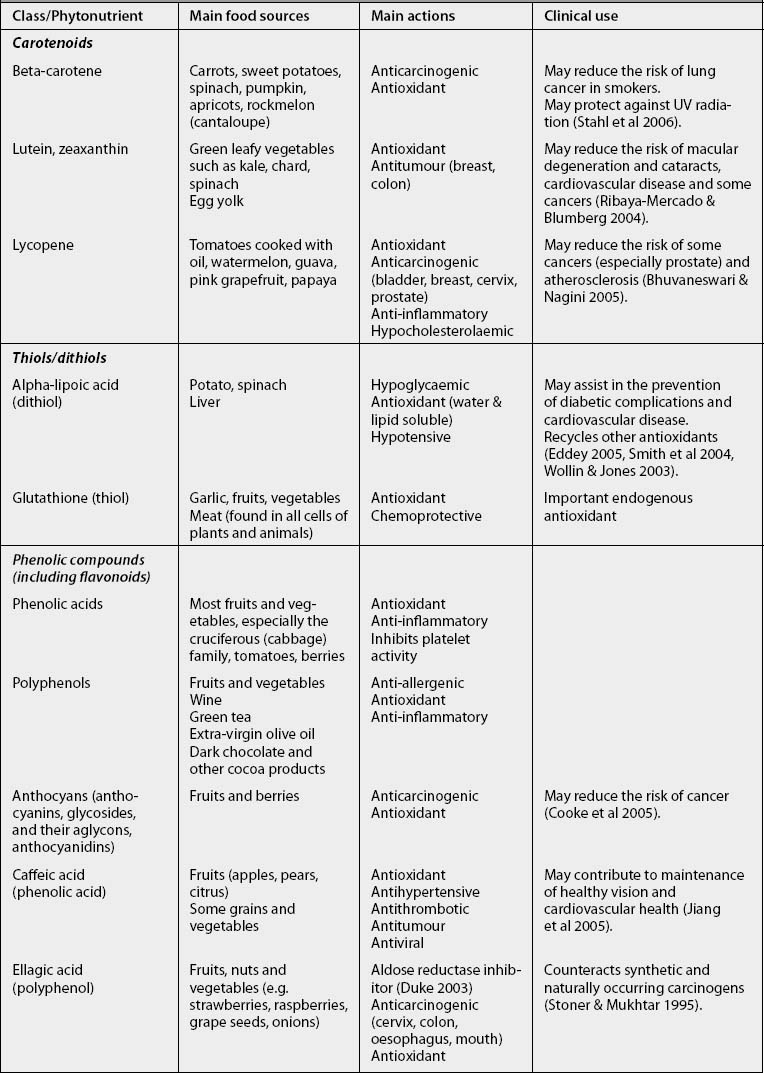
The foods and substances we ingest affect us even at the most basic cellular level. In recent years scientists have discovered many thousands of previously unidentified substances in food and described their therapeutic actions. Currently around 50,000 (of a likely 200,000 substances) have been identified and described, yet for the most part we know very little about their functions (Hounsome 2008). These substances are known as phytonutrients, phytochemicals or a-nutrients. They impart colour, taste and smell, as well as possessing therapeutic properties such as antioxidant, anticarcinogenic, antimicrobial, antihypertensive, anti-inflammatory and cholesterol lowering properties. Major classes of phytonutrients include phenolic and polyphenolic compounds (flavonoids, phenolic acids, lignins), terpenoids (carotenoids, tocopherols and tocotrienols, quinines, sterols), alkaloids (including saponins), and sulfur-containing compounds (glucosinolates) (Goldberg 2003). A brief summary of some of the better known phytonutrients, their major actions and therapeutic uses is shown in Table 5.1 (pp 48–50). Although thousands of studies have already been conducted to identify phytonutrients in foods and understand their properties and influence on human health, much remains unknown.
The concept of a ‘functional’ food originated in Japan and is now being further developed, mainly in Japan, the United States and Europe. Functional foods are foods or dietary components that provide a health benefit that goes beyond their nutritional value, such as improving wellbeing and/or reducing the risk of disease. These may include traditional foods that have been shown to impart a positive biological effect or foods that have been modified to impart health benefits. Other terms that are used for functional foods are super foods, designer foods, fortified foods, nutraceuticals, cosmaceuticals, medifoods, vitalfoods and Foods for Specified Health Use (FOSHU) (Ashwell 2002).
Functional foods can be foods in which a component has been enhanced through special growing conditions or foods in which a component has been added, removed, modified or had its bioavailability increased. Functional foods cannot be marketed as medicines because they cannot make therapeutic claims for treating specific diseases; rather they are designed to be marketed to healthy consumers to enhance health and prevent disease (Ashwell 2002). As such, functional foods are distinct from dietetic foods, which are designed for treating illness and are marketed to health professionals.
Examples of functional foods include yoghurt and probiotics, vitamin- and mineral-fortified breakfast cereals, iodised salt and sports drinks (which are proven to promote rapid gastric emptying and fast intestinal absorption, to improve water retention, thermal regulation and physical performance, and to delay fatigue) (Ashwell 2002). Many commonly prescribed ‘herbal medicines’ can also be considered as functional foods and are commonly used for both medicinal and culinary purposes. Many of these foods and food derivatives are included in the monographs in this book: for example, celery seed, chamomile, cloves, cranberry, dandelion, fenugreek, fish oils, garlic, ginger, green tea, honey, horseradish, lemon balm, licorice, linseeds, noni, oats, peppermint, probiotics, raspberry, rosemary, sage, stinging nettle, thyme and turmeric.
Although functional foods retain their identity as foods and do not include pills, the line between food and medicine is a fine one and the line between food and herbal medicine even finer. In Australia, foods (including herbal medicines) are regulated according to their intended use either by the TGA or by Food Standards Australia New Zealand (FSANZ 2006). Recently, recognition of the therapeutic value of foods has led to a review of the extension of permissible health claims, substantiated by scientific evidence, that are allowed on food packaging. Regulations currently allow for nutrient-content claims (e.g. ‘high in fibre’) and some health-maintenance claims. Other types of health claims, with the exception of claims about the benefit of maternal consumption of folate, are prohibited (FSANZ 2006).
Although the primary aim of altering foods to make them ‘functional’ is to promote their beneficial effects, consideration should also be given to the potentially negative implications of manipulating foods, such as altering the natural synergy of nutrients, the introduction of synthetic nutrients and the possibility of detrimental effects. In the USA, for example, mandatory fortification of cereal and grain products with folic acid has raised concerns about masking the haematological abnormalities of vitamin B12 deficiency, thereby allowing the progression of neurological complications to continue undetected (Rothenberg 1999), as well as placing some individuals at risk of exceeding the recommended safe upper limit of 1000 micrograms synthetic folate daily (Jamison 2005), while still failing to meet the peri-conceptual requirements of others (see Monographs: Folate).
SUPPLEMENTS VERSUS FOOD
The actions of a whole food cannot be completely understood by studying its various components in isolation, because phytonutrients often interact with one another and, when used together, can produce different outcomes from those predicted for an isolated compound. Thus supplementation with individual food components may produce different effects from those produced by the consumption of the whole food. For example, epidemiological studies supporting the use of foods containing beta-carotene for the prevention of lung cancer in smokers have not been supported by clinical trials of supplementation with synthetic beta-carotene (Ziegler et al 1996) (see Monographs: Beta-carotene). Similarly, there is strong evidence to suggest that eating a variety of fibre-rich foods is beneficial in the prevention and management of diabetes; however, studies using fibre supplements have produced contradictory results (Venn & Mann 2004).
INDIVIDUALISING FOOD
An old Chinese proverb states ‘Whatsoever was the father of disease, an ill diet was the mother’. Traditional medicine systems such as traditional Chinese medicine (TCM) and Ayurvedic medicine continue to understand and practise using food as medicine, and view food within a conceptual framework that includes the energetic value of food in addition to its physical qualities. An assessment of different foods may be based on the food’s ‘vitality’ or ‘life force’, otherwise known as ‘chi’ in TCM and ‘prana’ in Ayurvedic medicine. The type of food and its biological, nutritional and sensual properties, together with the many agricultural practices, production processes and preparation methods, make a contribution to this force. Every step in the process of producing a food may potentially affect the energetic value, net nutritional content and overall therapeutic benefits.
Biomedical science has not matched the same degree of sophistication in individualising diet as traditional medicines; however, it is moving in this direction. Just as in pharmaceutical medicine the emerging science of pharmacogenomics promises to provide drugs best suited to a person’s genetic makeup, the emerging science of nutrigenomics promises to deliver an understanding of how different nutrients affect genes to cause specific conditions and the ability to design foods and dietary recommendations based on an assessment of an individual’s genotype (see also Chapter 3).
The increasing individualisation, complexity and knowledge base of nutritional science has led to research into ‘Point-Of-Sale Individualised Foods’ (POSIFoods), which integrate advances in nutritional science, innovative food processing and formulation processes and state-of-the-art vending technology to deliver fast, palatable and nutritious foods, tailored to an individual’s dietary needs and taste preferences at the touch of a button (Decision News Media 2004). The success of such developments and their impact in human health, however, are yet to be determined.
FOOD QUALITY ISSUES
PESTICIDE RESIDUES
The creation of a global food industry and the emergence of agribusiness have led to the increasing use of pesticides in food production. At the same time there is growing worldwide public concern about the impact of these pesticides on human health. Currently, it is reasonable to expect that most animals on the planet have accumulated pesticide residues through water, air or the food chain and, although acute effects of pesticides are well documented, the chronic effects of pesticide exposure are more difficult to assess. A recent systematic review examined the peer-reviewed literature published between 1992 and 2003 on currently used pesticides (the ‘older’ organochlorine pesticides were excluded) and their effect on human health. The review found that there is a high level of consistency across multiple studies to indicate a wide range of pesticide-related clinical and subclinical health effects, including significant positive associations between pesticide exposure and solid tumours (such as cancers of the brain, breast, kidney, prostate and pancreas) and haematological cancers (such as non-Hodgkins lymphoma and leukaemia); genotoxic effects; as well as effects on mental and emotional functioning, the nervous system, neurodegenerative diseases and reproduction (including birth defects, fecundity, fetal death and intrauterine growth retardation) (Sanborn et al 2004). A further review of the effects of pesticides on children indicates that pesticide residues have been implicated in causing reproductive problems, including miscarriages and spontaneous abortion, birth defects, childhood cancer, and neurological, neurobehavioural and endocrine effects (Garry 2004).
Children’s exposure to pesticides may also be increased through breastmilk. This provides many immunological, physiological, nutritional and psychological advantages, but is nevertheless commonly contaminated with high levels of pesticides. For example, it has been found that serum concentrations of organochloride compounds are significantly higher (P < 0.0001) in breastfed infants than in bottle-fed infants (Lackmann et al 2004), and that an infant’s measured intake of organochlorines from breastmilk may greatly exceed the adult acceptable daily intake (ADI) (Quinsey et al 1995, 1996). In addition, children have less developed detoxification pathways; for example, newborn infants have low levels of the enzyme paraoxonase–1, which detoxifies organophosphate pesticides (Chen et al 2003). The fact that children born today have a longer life expectancy in which to develop diseases with long latency periods places them at further risk (Sanborn et al 2004). These factors led to the 1996 revision of the US Federal Fungicide, Insecticide and Rodenticide Act to include an additional 10-fold margin of safety for exposure to pesticide chemical residues in infants and children (Makris & Rowe 1998).
The dietary exposure of the Australian population to pesticides and other food contaminants was previously monitored every 2 years via the Australia Total Diet Survey (ATDS) conducted by Food Standards Australia New Zealand (FSANZ). The most recent surveys, however, have not included pesticides. The most recent to do so was the twentieth survey in 2003, which concluded that the levels of pesticide residues and contaminants found in Australian food sources were very low and within acceptable safety limits (FSANZ 2003a). The survey selected specific ‘contaminants’ for study and therefore cannot demonstrate broad effects on public health. Residue testing is also conducted on fresh produce in Australia (e.g. FreshTest and the National Residue Survey), but this is largely funded and directed by industry bodies.
Although safety assessments are conducted on pesticides and guidelines are set for maximum residue levels (MRLs), this does not necessarily guarantee food safety as numerous other factors need to be considered. Safety assessments usually examine only single chemicals at high doses and often only in animals, which may lead to a significant underestimation of the potential risk associated with the numerous mixtures of compounds that consumers are typically exposed to. The combined toxic effect of multiple chemicals is not necessarily predictable by adding up the toxic potential of each chemical; mixtures of chemicals can also interact to produce synergistic toxic effects. Thus it is possible that there may be greatly enhanced toxicity of these compounds when they are combined, and this is supported by research documenting reproductive, immune and nervous system effects not expected from the individual compounds acting alone (Boyd et al 1990, Porter et al 1993, 1999, Thiruchelvam et al 2000). Pregnant and lactating women require specific consideration to minimise exposure of the fetus or infant during critical periods of development, and children do not metabolise chemicals as efficiently as adults (Sanborn et al 2004).
GENETIC MODIFICATION (TRANSGENIC FOODS)
While advocates maintain that there is the potential for biotechnology to have a positive impact on the nutritional properties of transgenic foods and to allow for their cultivation in areas where farming is difficult, it has been argued that most transgenic foods have so far produced greater benefits for producers than consumers. Currently, only six countries (Argentina, Brazil, Canada, China, South Africa and the USA), four crops (corn, canola, cotton and soy) and two traits (herbicide tolerance and insect resistance) represent 99 per cent of the transgenic crops planted worldwide (FAO 2004): ‘The so-called “orphan crops” such as cowpea, millet, sorghum and teff that are critical for the food supply and livelihoods of the world’s poorest people’ and ‘traits of interest to the poor; drought and salinity tolerance, disease resistance, or enhanced nutrition’ are receiving little attention (FAO 2004). The prospect that transgenic crops could be used for mass medication and vaccination programs also raises concern in some circles.
Currently, six genetically modified (GM) foods have been approved for sale in Australia and New Zealand: all are derived from soybeans, sugar beet, corn, cottonseed oil, canola and potatoes. In Australia, to enable consumer choice, food producers are required to label foods that contain a GM-derived component or a GM protein introduced through genetic engineering; however, the genetic material that has been used is not specified. The introduction of these transgenic foods has been criticised, with claims that there is insufficient evidence of safety and that safety test technology is inadequate to assess potential harms (Pusztai 2001). It has also been suggested that a precautionary principle should be applied and that further research needs to be conducted on the possible health risks of transgenic foods before they are introduced (BMA 1999). In reality, the ultimate benefits and detriments of genetic engineering are unlikely to be known for several generations.
ANTIBIOTIC RESISTANCE
Approximately one-third of the antibiotics used in Australia are for human use. Two-thirds are used in intensive animal production, of which the majority is mixed into stockfeed to act as a growth promoter (JETACAR 1999). Furthermore, antibiotic resistance genes are sometimes added as marker genes to GM food. This has led to the fear that widespread antibiotic-resistant bacteria have emerged that can cause disease in humans and animals that will be difficult to treat. The British Medical Association has warned that antibiotic resistance is ‘one of the major public health threats that will be faced in the 21st century’ (BMA 1999), while the World Health Organization has called for a reduction in their use in agriculture (WHO 2001).
FOOD ADDITIVES AND IRRADIATION
Additives are listed as either numbers, known as additive codes, or by name; ‘de-coders’ are readily available in many bookstores. Up-to-date lists of the food additives used in Australian and New Zealand food products are freely available from FSANZ (2009). Additives include preservatives, artificial sweeteners, colourings and flavourings, monosodium glutamate, hydrogenated fats and phosphoric acid. Artificial colourings and preservatives in food and drink are thought to contribute to hyperactivity in some preschool children; although many still contest this issue, a recent study in the UK found that the proportion of hyperactive children halved when additives were removed from their diets (Bateman et al 2004).
A further concern is the long-term safety of consuming irradiated foods. Currently irradiation is used for the purpose of food preservation, to control microbes and to protect against critical quarantine pests. Irradiated food is exposed to gamma rays from a radioactive source, which kill insects, eggs, larvae and pathogenic microorganisms. This is an expensive procedure and thus is not extensively used in Australia at present. Currently the Food Standards Code in Australia allows for the irradiation of spices, herbs and herbal infusions, and tropical fruits (breadfruit, carambola, custard apple, lychee, longan, mango, mangosteen, papaya and rambutan) as a disinfestation measure for pests such as the fruit fly (FSANZ 2003b).
PROCESSING AND PREPARATION
While production and preservation methods may affect food quality, processing techniques may also significantly affect the therapeutic value of a food, and both benefits and detrimental effects are possible. For example, as both fibre and other nutrients are concentrated in the outer part of the grain, significant losses of not only fibre but also of B vitamins, fat-soluble vitamins and other nutrients occur when grain is refined (Jamison 2006). Similarly, food preparation methods can significantly affect a food’s therapeutic qualities. Consider the potentially different nutritional and energetic effects of the same food consumed raw, juiced, steamed, boiled, fried, barbecued or microwaved. The microwaving of broccoli, for instance, has been found to destroy 97% of the flavonoids; conventional boiling destroys 66% and high-pressure boiling causes considerable leaching into the cooking water, whereas steaming produces minimal loss (Vallejo et al 2003).
Cooking does not always have detrimental effects and can sometimes increase the bioavailability of bioactive compounds; for example, the lycopene in tomatoes is more bioavailable when tomatoes are cooked in oil. The concentration of phenolic compounds in a food may also be increased by thermal processing, resulting in a significant increase in overall antioxidant status, despite some loss of heat-sensitive antioxidant nutrients such as vitamin C (Jamison 2006).
Food combination is another factor that influences the therapeutic value of a meal; for instance, consuming red meat with leafy greens and a citrus salad dressing synergistically improves iron absorption. The consumption of antioxidants in the diet, such as the tocopherols, coenzyme Q10, carotenoids, vitamin A, ascorbic acid, reduced glutathione, selenomethionine, flavonoids and other polyphenolic compounds, together with spices and synthetic antioxidants added to food, counteract the effects of pro-oxidants found in food and the environment. Applying this concept, it could be suggested that foods containing high levels of pro-oxidants (e.g. meat) should be served with plenty of antioxidant-containing vegetables, together with sauces, juices, fruits and teas high in antioxidants (Surai et al 2004). This is supported by a study of 2814 male smokers who participated in the Belgian Interuniversity Research on Nutrition and Health study. This found that men with the highest oxidative balance score had a higher relative risk of all-cause mortality (RR = 1.44, 95% confidence interval [CI]: 1.13, 1.82) and of total cancer mortality (RR = 1.62, 95% CI: 1.07, 2.45), compared with men in the lowest-score group (Van Hoydonck et al 2002).
Glycaemic index™
Observational studies indicate that a low-GI diet reduces elevated low-density lipoprotein (LDL) and triglyceride levels, raises high-density lipoprotein (HDL) levels (Dushay & Abrahamson 2005), and improves fasting glucose and glycated protein values (Anderson et al 2004).
Social, cultural and environmental aspects
In addition to being influenced by physico-chemical properties, the therapeutic qualities of food may further be affected by a person’s psychological state and/or intention while preparing and eating food, as well as by the social, cultural, economic, ethical, religious and environmental impact of the food. It has been said that ‘eating is essentially an act of communion with the living forces of nature’ (Robbins 1992). Indeed, most cultures and traditions have developed mealtime rituals that acknowledge the source of their food and attempt to align mind and body with the greater forces of nature. Food also features prominently in many spiritual traditions and practices. Thus, the idea of saying grace before meals and then eating ‘gracefully’ and mindfully, without rushing, may make significant contributions to psychological and spiritual health.
Food and health are both multidimensional and interrelated. Food choices not only influence physiological functioning, but have much broader social, economic, ethical and environmental ramifications, which may in turn affect personal health and wellbeing. Some of these aspects are becoming acknowledged in wider food-related social movements, such as the Fair Trade Federation (see www.fairtradefederation.org), International Slow Food Movement (see www.slowfood.com) and Food Miles (see Sustainable Agriculture–Food and Environment Alliance (SAFE), (see www.sustainweb.org).
Food is not just a means of providing nutrition and sustaining health, it is also a global industry that affects everyone. In the new global economy, there is a fear that the production, trade and retailing of most goods and services are being increasingly concentrated under the control of a small number of corporations that have enormous influence. It is questionable whether all corporations take sufficiently seriously the responsibility of providing quality foods while protecting workers and their environment, and whether free-trade agreements do any more than just offer global protection for a company’s intellectual and property rights. For example, global trade in coffee and cocoa has led to social disruption, environmental damage and the mistreatment of workers, including children, who earn meagre wages while corporations make huge profits (Cavanagh 2002).
To counter this trend, the Fair Trade Federation (www.fairtradefederation.org) sets standards for commodities, such as coffee, tea, sugar, cocoa and fruits, that will support living wages and safe, healthy conditions for workers in the developing world. Fair Trade standards stipulate that traders must pay a price to cover the costs of sustainable production and living, and the organisation attempts to support food-producing communities by paying a premium that producers can invest in development, making partial advance payments when requested by producers and signing contracts that allow for long-term planning and sustainable production practices.
The interests of the food industry and agribusiness are not always aligned with the interests and needs of consumers; for example, the widespread availability of fast foods and their enormous popularity threatens gastronomic traditions, traditional cultivation and processing techniques, while standardising taste. The Slow Food Movement is an international movement that originated in Italy; it attempts to address these concerns by:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree