III. Intravenous Fluid Types
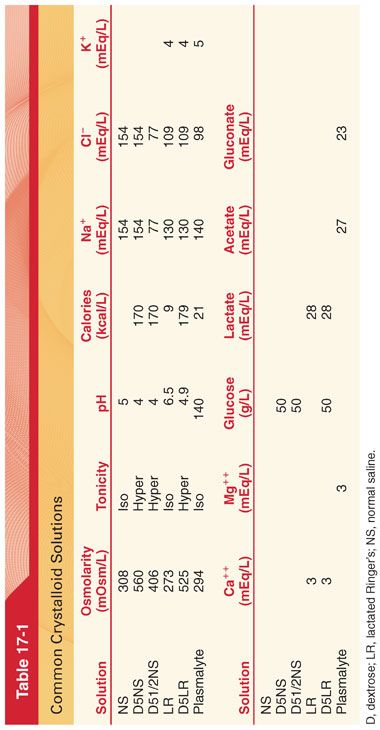
A. Crystalloids are fluid solutions containing ion salts and other low-molecular-weight substances (categorized based on their tonicity or osmotic pressure of the solution with respect to that of plasma) (Table 17-1). Administering large volumes of normal saline can result in hyperchloremic metabolic acidosis. “Balanced” or “physiologic” crystalloid solutions contain a composition approximating that of extracellular fluid but are usually slightly hypotonic because of lower sodium concentration.
B. Colloids (Table 17-2)
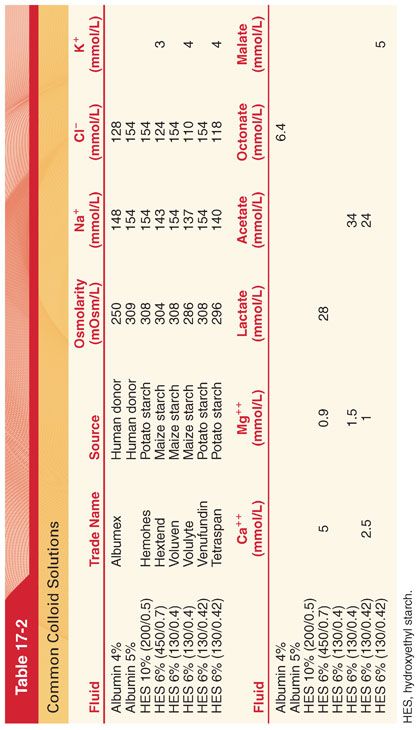
1. Albumin (4% to 5%) solution is produced from human blood and suspended in saline (heat-pasteurized at 60°C for 10 hours to reduce viral transmission). It is expensive to produce and distribute as compared to semisynthetic colloids and crystalloid solutions. The comparative effectiveness of fluid resuscitation with colloid versus crystalloid has been a long-standing controversy (studies show no difference in survival).
2. Semisynthetic colloid solutions (hydroxyethyl starch solutions [HES], succinylated gelatin, urea-linked gelatin–polygeline preparations, dextran solutions) (Table 17-3).
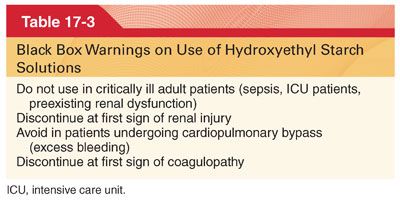
a. HES is the most commonly used semisynthetic colloid solution.
b. The maximum daily dose of HES is limited to 20 to 50 mL/kg of body weight/day but varies by solution.
c. HES is removed from the circulation by redistribution and renal excretion.
d. HES compounds have effects on coagulation with reductions in factor VIII, von Willebrand factor, and platelet function (noted even when used below recommended maximum doses). Solutions with more rapid degradation are associated with less effects on coagulation.
e. The incidence of anaphylactoid reactions with HES use is 0.085%.
f. When compared with saline, HES was associated with significantly more adverse events.
IV. Assessing Fluid Responsiveness
A. Fluid responsiveness may be defined as a 15% increase in cardiac output following a 500-mL intravenous (IV) fluid bolus, indicating that the patient is still on the ascending limb of the cardiac output/end diastolic volume curve, also referred to as the cardiac function curve. Fluid administration to a patient on the plateau part of the curve may be of little benefit and result in adverse effects.
B. Filling pressure measures, particularly central venous pressure, correlate poorly with blood volume, and changes in central venous pressure have been shown to poorly predict hemodynamic response to fluid challenge. Stroke volume changes due to increases or decreases in right ventricular preload may be used to assess fluid responsiveness.
V. Important Fluid Constituents
A. Magnesium. Plasma magnesium level is normally 1.7 to 2.4 mg/dL and measurements may not be representative of total body magnesium stores (magnesium measurements can be falsely elevated with hemolysis of the blood sample, which releases the intracellular electrolytes). Excretion occurs via the kidney with more than 95% of the filtered magnesium being reabsorbed in the renal tubules, with this mechanism effectively regulating the plasma level.
1. Role of Magnesium
a. Magnesium plays a key role in many biologic processes including protein synthesis, neuromuscular function, and nucleic acid stability.
b. Magnesium has antiarrhythmic properties related to calcium channel antagonism. IV magnesium administration can exert muscle-relaxing effects, enhance nondepolarizing neuromuscular blockers, attenuate muscle fasciculations and potassium release with administration of succinylcholine, and precipitate skeletal muscle weakness in patients with Lambert-Eaton syndrome and myasthenia gravis. It has been used to reduce anesthetic requirements and attenuate cardiovascular effects of laryngoscopy and intubation. Magnesium decreases blood–brain barrier disruption and limits cerebral edema formation after brain injury.
c. Side effects of IV administration include muscle weakness, hypotension, and bradycardia.
2. Hypomagnesemia may result from dietary deficiency (chronic alcoholism), gastrointestinal malabsorption or secretion (diarrhea, vomiting, laxative use), renal losses (medication effects, nephrotoxic agents, endocrine disease, diabetic nephropathy), and chelation (citrate binding in the case of massive transfusion).
a. Hypomagnesemia is seen in as many as 11% of hospitalized patients and 65% of patients in the intensive care unit.
b. Clinical manifestations of hypomagnesemia include cardiac and neuromuscular disorders, electrocardiogram (ECG) abnormalities (prolonged PR and QT intervals, diminished T-wave morphology, torsades de pointes), and accompanying hypokalemia and hypocalcemia.
3. Hypermagnesemia is rare and most commonly occurs with excessive administration of magnesium for therapeutic purposes.
a. Clinical manifestations include QRS widening, hypotension, narcosis, diminution of deep tendon reflexes, respiratory depression from paralysis of muscles of ventilation, heart block, and cardiac arrest.
b. Immediate treatment of life-threatening hypermagnesemia is with calcium gluconate, 10 to 15 mg/kg IV, followed by diuretics or dialysis, along with appropriate respiratory and circulatory support.
4. Preeclampsia
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


