Intravascular Large B-cell Lymphoma
Francisco Vega, MD, PhD
Key Facts
Terminology
Rare large B-cell lymphoma characterized by selective intravascular growth
Clinical Issues
Heterogeneous clinical signs: Nodules/plaques (49%), macules (23%), telangiectatic patches (20%)
Absence of marked lymphadenopathy
Middle-aged or elderly patients
Neurologic and dermatologic manifestations common
Patients from Asia often show hemophagocytic syndrome
Cutaneous variant
Most frequent in females, usually younger patients
Better prognosis (3-year survival rate of 56%, systemic variant: 22%)
Microscopic Pathology
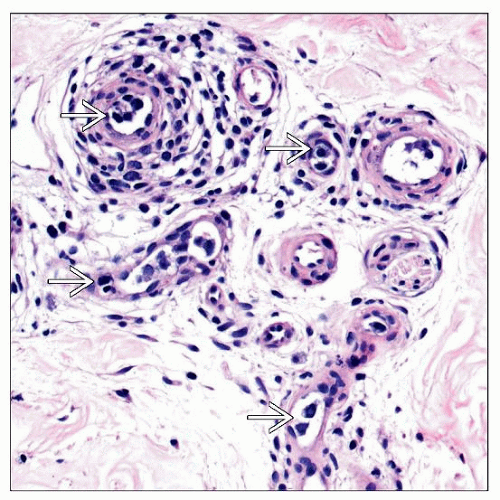
IVLBCL cells are large, with vesicular nuclear chromatin, distinct nucleoli, and frequent mitoses
Lymphoma cells are mainly located in lumina of small vessels
Ancillary Tests
Pan-B-cell markers (+), Bcl-2(+), MUM1(+)
CD5(+) (30%); other T-cell markers (−)
Ki-67 high
Top Differential Diagnoses
Peripheral T- or NK-cell lymphomas with intravascular pattern
Hepatosplenic T-cell lymphoma
T-cell large granular lymphocytic leukemia
Diffuse large B-cell lymphoma, NOS
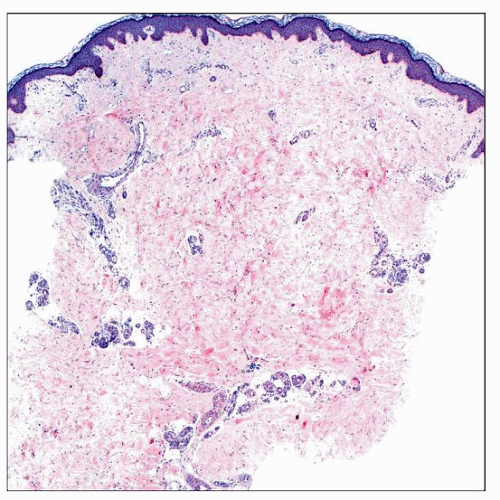 Intravascular large B-cell lymphoma (IVLBCL) involving skin is shown. Note that the infiltration by neoplastic cells is difficult to recognize at this low magnification. |
TERMINOLOGY
Abbreviations
Intravascular large B-cell lymphoma (IVLBCL)
Synonyms
Angiotropic large cell lymphoma
Angioendotheliotropic (intravascular) lymphoma
Intravascular lymphomatosis
Definitions
Large B-cell lymphoma characterized by selective intravascular growth
Preferential intravascular growth is a condition sine qua non for diagnosing IVLBCL
Concomitant and minimal extravascular location of neoplastic cells, usually surrounding involved vessels, can be seen
CLINICAL ISSUES
Site
Selective tumor growth within lumina of small blood vessels, particularly capillaries
Widely disseminated
Any organ can be involved
Absence of marked lymphadenopathy
Mechanisms responsible for selective growth of neoplastic cells within blood vessel lumina are unknown; possible explanations include
Chemokine-chemokine receptor interactions
e.g., CXCL9 (expressed in endothelium) and CXCR3 (expressed in IVLBCL)
Decreased expression of adhesion molecules on surface of IVLBCL cells
e.g., CD29 and CD54
Presentation
Middle-aged or elderly patients; median: 67 years
M:F ratio = 1.3:1
IVLBCL can involve any organ with heterogeneous, often nonspecific symptoms
Fever of unknown origin
General fatigue
Deterioration in performance status
Diagnosis can be clinically difficult and some cases are diagnosed postmortem
2 major patterns of clinical presentation
Western IVLBCL
Predominant neurologic and dermatologic manifestations
Central nervous system is involved in most patients
Asian IVLBCL
Hemophagocytic syndrome
Fever and B symptoms
Pancytopenia and bone marrow infiltration
Skin and central nervous system involvement are uncommon
Skin
Heterogeneous clinical presentation: Nodules/plaques (49%), macules (22.5%), telangiectatic patches (20%), cellulitis, ulcerated nodules
Waxing and waning lesions (16%)
Lower and upper extremities, trunk and lower abdomen
Skin involvement is sometimes detected by random skin biopsy of grossly unremarkable skin
Cutaneous variant
Most frequent in females
Younger than other IVLBCL patients
Usually not associated with leucopenia or thrombocytopenia
Better prognosis (3-year survival rate of 56%, systemic variant: 22%)
Kidney
Increased creatinine
Proteinuria
Renal insufficiency
Liver
Hepatomegaly
Increased bilirubin and liver enzymes
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree