Intraoperative Parathyroid Hormone Assay–Guided Parathyroidectomy
Carmen C. Solorzano
Denise M. Carneiro-Pla
John I. Lew
Introduction
The ability to quickly measure parathyroid hormone (PTH) in plasma and tissue has changed the understanding and surgical management of sporadic primary hyperparathyroidism (SPHPT). This disease entity is the result of autonomous hypersecretion of PTH by one or more parathyroid glands. Surgical treatment of SPHPT continues to be based on the identification and removal of all hypersecreting parathyroid tissue while preserving normally functioning glands that maintain calcium homeostasis. There are currently two major operative approaches: traditional parathyroidectomy and focused parathyroidectomy. The majority of high-volume parathyroid surgeons perform focused parathyroidectomy guided by preoperative localization studies and intraoperative parathyroid monitoring (IPM).
In this chapter, the use of IPM as an adjunct during parathyroidectomy in patients with SPHPT is discussed.
In this chapter, the use of IPM as an adjunct during parathyroidectomy in patients with SPHPT is discussed.
Traditional parathyroidectomy requires bilateral neck exploration (BNE) that involves the identification of usually four parathyroid glands, and based on the surgeon’s judgment, the excision of all grossly enlarged glands. All normal-sized parathyroid glands are left in situ. A problem with this approach is that the size of a parathyroid gland does not always directly correlate to its secretory function. If any hypersecreting gland(s) is left behind, hypercalcemia will persist, resulting in a failed parathyroidectomy. Conversely, if too many normally functioning parathyroid glands are excised or their blood supply compromised during extensive dissection, postoperative hypoparathyroidism with resultant hypocalcemia and tetany may occur. Large series have shown that this operative approach yields success rates of 95% to 99% when performed by experienced parathyroid surgeons. However, these curative rates may fall to 70% when traditional parathyroidectomy is performed by inexperienced surgeons.
In the early 1990s, imaging studies were increasingly being used by surgeons to localize and guide parathyroidectomy. Unfortunately, these localization studies frequently missed multiple gland disease (MGD) making them unreliable as the sole adjunct to focused parathyroidectomy. Around this time, IPM was introduced precisely to avoid missed MGD and to assure complete excision of all hypersecreting glands before leaving the operating room. Since its introduction more than a decade ago, IPM has transformed the surgical management of SPHPT from traditional BNE to a more focused, less invasive parathyroidectomy requiring minimal neck dissection.
Candidates for Ipm-Guided Parathyroidectomy
Parathyroidectomy should be considered in a patient with a secure diagnosis of SPHPT shown by (a) persistent hypercalcemia, (b) elevated PTH level, (c) normal renal function, (d) normal or elevated urinary calcium, and (e) no history of multiple endocrine neoplasia. Excellent operative success can be achieved in most patients with symptoms associated with hypercalcemia or in those patients with no apparent symptoms and surgical indications as detailed by the Summary Statement from the Third International Workshop on the Management of Asymptomatic Primary Hyperparathyroidism in 2008.
History of Ipm
Reiss and Canterbury first described an antibody with good affinity for PTH in humans using an immunoradiometric assay. The utility of this assay, however, was limited as it recognized only part of the PTH molecule. In 1987, Nussbaum and colleagues described a new method for measuring the intact (1–84) PTH molecule by using a two-site antibody technique that proved more sensitive and specific than previous PTH assays. Since PTH has a rapid rate of decay (half-life, 3 to 5 minutes), these authors suggested that intraoperative measurement of PTH might prove useful to the surgeon performing parathyroidectomy. The impetus for developing a quick quantitative method to determine the removal of all abnormal parathyroid tissue was a hypersecreting parathyroid gland that was missed after excision of a single enlarged gland during BNE. In 1990, Irvin and colleagues refined and applied this assay to routine clinical practice in the surgical management of SPHPT at the University of Miami. By heating and shaking the antibodies with the patient’s blood sample to speed reaction times using this assay, intraoperative PTH monitoring (IPM) was shown to predict postoperative normocalcemia in patients after parathyroidectomy. With the later transition from radionuclear to immunochemiluminescent technology, this PTH assay became a practical test for intraoperative, point-of-care use. Since 1996, rapid PTH assays have become commercially available for intraoperative use, and such surgical adjuncts are now used worldwide.
How Ipm Works
IPM is used by surgeons to confirm the complete excision of all hyperfunctioning parathyroid tissue. The surgical adjunct also alerts the surgeon of an incomplete removal of abnormal parathyroid tissue, thereby indicating the need for further exploration. Currently, hypersecretion of PTH by abnormal gland(s) is measured by a nonradioactive two-site immunochemiluminescent antibody that captures and quantifies the unknown amount of hormone in a sample of plasma. Rapid results are essential if the surgeon is to use hormone dynamics to guide parathyroidectomy. Most intraoperative assays provide results on an average of 8 to 20 minutes, and the PTH dynamic changes shown by these rapid assays correlate well with standard diagnostic assays with respective normal ranges. Since surgeons need a short turnaround time, point-of-care capability with the assay equipment placed in, or in close vicinity to, the operating room is of utmost importance.
Table 1 Definitions Used to Calculate the Accuracy of the “>50% PTH Drop” Criterion in Predicting Postoperative Calcium Levels for at Least 6 Months After Parathyroidectomy | ||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||
How Ipm Is Used
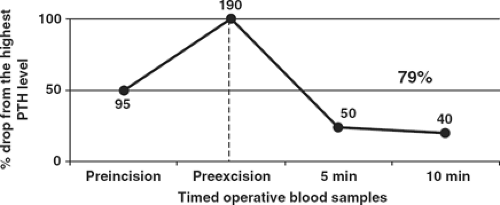
IPM only measures the circulating amount of hormone at the time and from the location where the sample is obtained. The surgeon must be attentive, understand, and direct the sampling times related to the stages of the operative procedure. There are several intraoperative criteria published that predict postoperative calcium levels using changes in hormone dynamics following excision of hyperfunctioning glands. The initially described criterion used to predict postoperative eucalcemia in patients with SPHPT is a “>50% PTH drop” 10 minutes after complete resection of all hyperfunctioning tissues (Table 1). This protocol developed at the University of Miami by George L. Irvin III requires peripheral venous or arterial access for blood collection at specific times during parathyroidectomy. This intravenous access is kept open with a slow infusion of saline, which must be discarded from the line before any blood sample is measured to prevent dilution. During the procedure, the anesthesiologist collects 4 mL of whole blood in an EDTA tube at specific times: (a) a “preincision” level before skin incision, (b) a “preexcision” level collected after dissection and just before
clamping the abnormal gland’s blood supply, (c) a 5-minute level, and (d) 10-minute level after excision of the suspected abnormal gland. When peripheral PTH values drop more than 50% from the highest either preincision or preexcision level 10 minutes after the excision of all abnormal parathyroid gland(s), this criterion predicts normal or low calcium levels postoperatively with an overall accuracy of 98%. After this sufficient decrease occurs, the observed hormone dynamic guides the surgeon to terminate the procedure without further exploration or identification of the remaining normally secreting parathyroid glands. An example of IPM used in a patient after excision of a single hypersecreting gland is shown in Figure 1. With an adequate PTH drop at the 10-minute postexcision interval from the highest preincision or preexcision PTH level, this hormone dynamic predicts a postoperative return to eucalcemia without further exploration of the remaining glands. IPM does not predict late recurrence of hyperparathyroidism (following at least 6 months of eucalcemia), but only that all currently hypersecreting glands have been excised.
clamping the abnormal gland’s blood supply, (c) a 5-minute level, and (d) 10-minute level after excision of the suspected abnormal gland. When peripheral PTH values drop more than 50% from the highest either preincision or preexcision level 10 minutes after the excision of all abnormal parathyroid gland(s), this criterion predicts normal or low calcium levels postoperatively with an overall accuracy of 98%. After this sufficient decrease occurs, the observed hormone dynamic guides the surgeon to terminate the procedure without further exploration or identification of the remaining normally secreting parathyroid glands. An example of IPM used in a patient after excision of a single hypersecreting gland is shown in Figure 1. With an adequate PTH drop at the 10-minute postexcision interval from the highest preincision or preexcision PTH level, this hormone dynamic predicts a postoperative return to eucalcemia without further exploration of the remaining glands. IPM does not predict late recurrence of hyperparathyroidism (following at least 6 months of eucalcemia), but only that all currently hypersecreting glands have been excised.
Conversely, if the hormone level fails to drop at the 10-minute interval following excision of a suspected hyperfunctioning parathyroid gland, the PTH assay signals that more hypersecreting tissue is likely to be present. Thus, the surgeon is directed to continue the exploration with the above described protocol applied to each removed gland. Another example of IPM shows the hormone dynamics in a patient with multiple gland disease (MGD) in Figure 2.
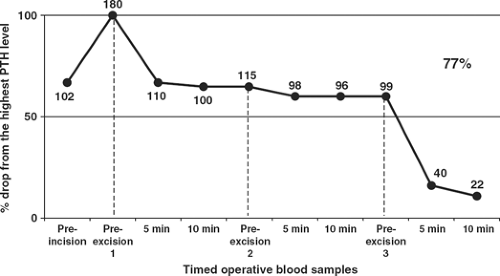 Fig. 2. Intraoperative parathyroid hormone (PTH) dynamics during successful parathyroidectomy in a patient presenting with multiglandular disease (MGD). An intraoperative preincision level of 102 pg/mL, careful dissection of an abnormal right inferior parathyroid gland led to a rise of PTH level to 180 pg/mL. After excision of this hypersecreting gland, the PTH assay showed no decrease at 5 minutes (110 pg/mL) and 10 minutes (100 pg/mL). Reexploration of the neck revealed two additional abnormal hypersecreting glands. The fourth gland appeared grossly normal. This graph shows that the expected hormone level did not decrease significantly until excision of the third hyperfunctioning parathyroid gland. With a 77% decrease in the 10-minute sample (22 pg/mL) compared with the third preexcision plasma sample (99 pg/mL), no remaining hypersecreting parathyroid tissue was present.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|