Intraoperative Cholangiogram
Chasen A. Croft
Dawood G. Dalaly
DEFINITION
Intraoperative cholangiography (IOC) is the use of radiography with contrast media injected directly into the biliary tree to determine biliary anatomy, assess the biliary tree for obstructive processes, and to evaluate for potential injury to the biliary tract.
PATIENT HISTORY AND PHYSICAL FINDINGS
Many surgeons routinely perform cholangiography as a part of every cholecystectomy. Others selectively use cholangiography based on the results of preoperative testing or intraoperative findings. A preoperative common bile duct (CBD) diameter greater than 6 mm, obstructive jaundice (direct bilirubin >4.0 g/dL), pancreatitis, and small stones in the gallbladder have all been forwarded as indications for IOC. Intraoperative indications would include palpating stones in the CBD, unclear biliary anatomy, or to evaluate for inadvertent injury to the biliary tree.1
IMAGING AND OTHER DIAGNOSTIC STUDIES
Prior to proceeding with cholecystectomy with IOC, patients should have an ultrasound evaluation of their biliary tree to assess for cholelithiasis, cholecystitis, and to determine the diameter of the extrahepatic CBD. Note that abdominal ultrasound is not a sensitive indicator of choledocholithiasis as CBD gallstones are often located in the distal CBD within the intrapancreatic portion and are thus obscured by air in the overlying stomach and/or are beyond the depth of penetration of ultrasound.
In the absence of cholangitis, but presence of ultrasound or laboratory findings suggestive of choledocholithiasis, one forwarded option is to preoperatively evaluate the biliary tree with magnetic resonance cholangiopancreatography (MRCP) to determine the cause of biliary tree obstruction. Should biliary obstruction be present, preoperative endoscopic retrograde cholangiopancreatography (ERCP) is then performed to clear the duct of stones prior to cholecystectomy or identify more ominous etiologies of the biliary obstruction.
Alternatively, others have advocated directly proceeding to cholecystectomy with IOC in this clinical setting, arguing that current modalities lack accuracy in identifying clinically significant choledocholithiasis and performance of an IOC often clears the duct of small stones. As such, these surgeons argue that the presurgical probability that an ERCP is necessary is low and this approach is more cost-effective by avoiding unnecessary ERCP.
SURGICAL MANAGEMENT
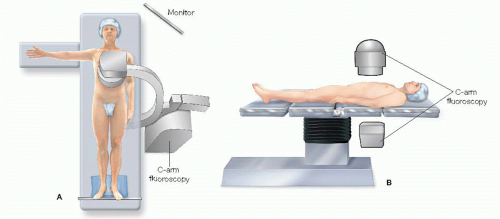
Positioning
The patient should be placed in the supine position on the operating room table. The left arm is preferentially tucked against the torso to provide room for C-arm fluoroscopy. The table should be positioned with respect to the supporting pedestal so as to allow the fluoroscopy C-arm to slide underneath the operating table unobstructed (FIG 1).
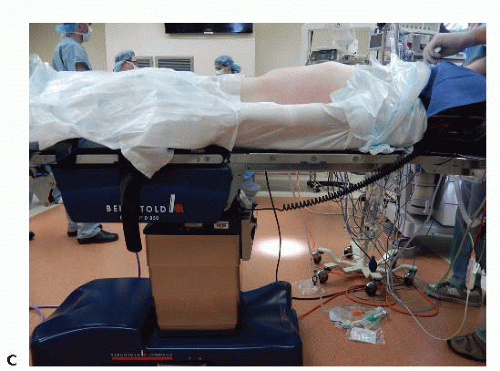
FIG 1 • (continued) C. Photograph demonstrating a clear path beneath the abdomen of the patient for the C-arm.
The C-arm fluoroscopy unit should be positioned to the patient’s right with the screen monitor clearly visible to the operating surgeon.
The bed should have a footboard placed and the patient should be well secured to the operating table, as reverse Trendelenburg position is required during the procedure.
Radiation Safety
The surgeon must be knowledgeable in the use of fluoroscopy. This should include successful completion of institutional training including certification for use of fluoroscopy in the operating theater.
All operating room personnel should don appropriate protective garments prior to scrubbing and gowning.
TECHNIQUES
CHOLANGIOCATHETER PLACEMENT
Cystic duct approach
The gallbladder infundibulum should be mobilized and dissection of Calot’s triangle should identify the cystic duct and artery entering the infundibulum.
Once the cystic duct is circumferentially dissected, a clip should be placed across the cystic duct as proximal as possible to the infundibulum (FIG 2).
A ductotomy should be made along the cystic duct, leaving adequate length for subsequent double clip ligation. Care must be taken to avoid fully transecting the duct with this maneuver. An intact posterior-cephalad cystic duct wall is essential to maintain exposure and facilitate placement of the cholangiogram catheter (FIG 3). Note that it is typical for the ductotomy to enlarge with the necessary lateral retraction to provide exposure or with manipulation with the cholangiogram catheter. Furthermore, the skeletonized cystic duct typically lacks intrinsic strength and can tear easily with aggressive retraction once a ductotomy has been made.
Two techniques for placement of the cholangiocatheter for laparoscopic IOC have been described:
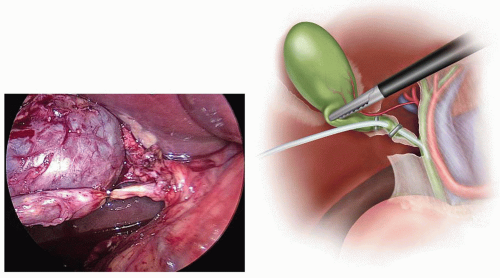
FIG 2 • After circumferential dissection of the cystic duct, a clip is applied at the junction with the infundibulum.
The first technique employs a 5-Fr cholangiocatheter inserted through an introducer sheath (FIG 4). This sheath, available as a component
of commercially available cholangiogram catheter kits, is inserted through a separate incision along the right subcostal margin. Placement of this incision should be guided by location of the ductotomy. Ideally, the catheter enters the abdomen lateral and caudad to the cystic duct (FIG 5).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree