Inflammatory Pseudotumor-like Follicular Dendritic Cell Tumor
Roberto N. Miranda, MD
Key Facts
Terminology
Inflammatory pseudotumor-like follicular dendritic cell tumor (IPT-FDCT)
Considered variant of follicular dendritic cell sarcoma
Classification is controversial
Clinical Issues
Marked female predominance
Good prognosis; no deaths attributable to IPT-FDCT of spleen
IPT-FDCT affecting liver can be recurrent and metastatic in rare cases
Microscopic Pathology
Well-demarcated single mass with occasional incomplete fibrous capsule
Loosely aggregated or dispersed oval or spindle cells admixed with abundant inflammatory cells
Ancillary Tests
Usual reactivity with follicular dendritic cell markers
Epstein-Barr virus encoded RNA (EBER)(+) in spindle cells in 40% of cases
Cases that are EBV(+) show that viral genome is monoclonal
Top Differential Diagnoses
Splenic inflammatory pseudotumor
Follicular dendritic cell sarcoma
Inflammatory myofibroblastic tumor
Sclerosing angiomatoid nodular transformation of red pulp
TERMINOLOGY
Abbreviations
Inflammatory pseudotumor-like follicular dendritic cell tumor (IPT-FDCT)
Synonyms
Terms inflammatory pseudotumor and inflammatory myofibroblastic tumor have been used as synonyms in the literature
This is confusing and may be incorrect
In this chapter these entities are distinguished
Definitions
IPT-FDCT is considered a variant of follicular dendritic cell sarcoma
Classification is controversial since several entities were previously lumped into category of splenic IPT
IPT-FDCT
True neoplasm of low malignant potential
Frequent association with Epstein-Barr virus (EBV)
Tends to involve spleen &/or liver
May overlap with EBV(+) cases without follicular dendritic cell markers
ALK(+) inflammatory myofibroblastic tumor (IMT)
Most often involves soft tissues of children and young adults
˜ 50% of tumors have rearrangements at 2p23 involving anaplastic lymphoma kinase (ALK)
Splenic inflammatory pseudotumor (IPT)
Reactive process composed of admixed bland spindle cells and inflammatory cells
Probably results from multiple etiologies, including infections and repair
Benign lesions that do not recur after surgical excision
ETIOLOGY/PATHOGENESIS
Infectious Agents
Etiology is unknown
Strong association with Epstein-Barr virus
Epstein-Barr virus is monoclonal when assessed by EBV DNA terminal repeat regions
Cell of Origin
Spindled cells express 1 or more follicular dendritic cell markers
Spindled cells also can express focally smooth muscle actin or S100 protein
Cell of origin may be mesenchymal cell with differentiation along fibroblastic, myofibroblastic, or follicular dendritic cell lineages
CLINICAL ISSUES
Epidemiology
Incidence
Uncommon; ˜ 1% of splenic tumors
Rare when compared with IPT at other sites of body
Age
Median: 44 years (range: 19-87 years)
Rare in children
Gender
Female predominance
Site
Appears in spleen as single lesion
Presentation
Affected patients are immunocompetent
Fever and weight loss in approximately 1/2 of patients
Epigastric or left flank pain in subset of patients
Splenomegaly may be noted in some cases
Can be incidental finding in asymptomatic patients
Lesion in spleen detected by radiologic imaging performed for other diseases
Imaging studies can demonstrate significant tumor growth in patients followed with less than 1 year intervals
Laboratory Tests
Usually unremarkable when not associated with other disease
Natural History
Cases of splenic IPT-FDCT appear to be closely related to liver IPT-FDCT
Histologically similar
Share association with EBV
More clinical information and follow-up are available for liver IPT-FDCT
Recurrences and metastases have been reported
Rare transformation of IPT-FDCT into overt follicular dendritic cell sarcoma
Treatment
Patients usually are diagnosed/treated with splenectomy
Due to rarity and nonspecific CT or MR imaging, these tumors are not diagnosed preoperatively
Symptoms and any laboratory abnormalities disappear after tumor resection
Prognosis
Good; no deaths attributable to IPT-FDCT of spleen
IMAGE FINDINGS
CT Findings
Discrete, single splenic mass and occasional splenomegaly
Lymphadenopathy is unusual
MACROSCOPIC FEATURES
General Features
Spleen weight: Ranges from 140-1,030 g
Well-circumscribed single mass
Cut surface is tan, gray, and firm; bulges in cross section
May have focal necrosis
Size: Ranges from 3-22 cm
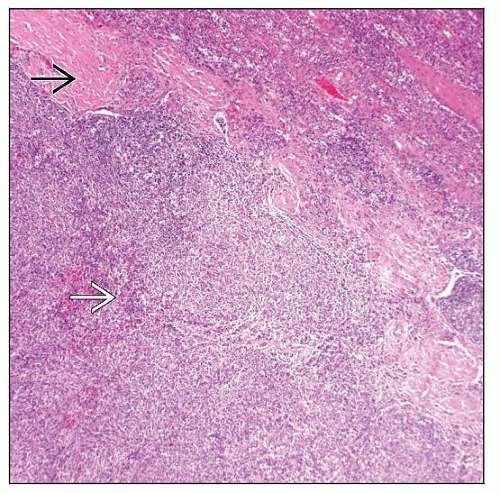
MICROSCOPIC PATHOLOGY
Histologic Features
Well-demarcated tumor with occasional incomplete fibrous capsule
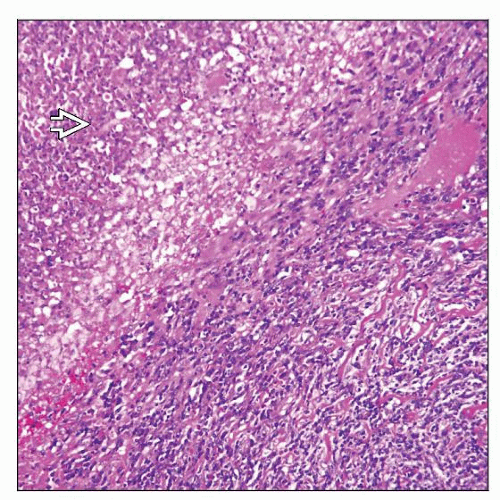
Loosely aggregated or dispersed oval or spindle cells admixed with abundant inflammatory cells
Spindled cells with moderate amount of pale to faintly eosinophilic cytoplasm
Oval vesicular nuclei with minimal atypia and distinct small nucleoli
Occasional small fascicles or focal storiform pattern
Rare mitotic figures
Occasional large cells with abundant cytoplasm and pleomorphic nuclei
Mixed inflammatory infiltrate of plasma cells, lymphocytes, and histiocytes
Lymphocytes are usually small admixed with occasional immunoblasts
Mature plasma cells with occasional Russell bodies
Other microscopic features
Focal necrosis with neutrophilic infiltrate
Histiocytes &/or eosinophils can be numerous
ANCILLARY TESTS
Immunohistochemistry
Spindled cells
Usually focal and weak reactivity with 1 or more follicular dendritic cell markers
CD21, CD35, CNA.42 (more frequent), and CD23 (less frequent)
More studies needed to establish frequency, pattern, intensity of expression of these markers
Vimentin(+), focal CD68(+), and focal smooth muscle actin(+/-)
Occasionally S100 protein ([+] focal)
EBV LMP1 occasionally (+)
Negative for CD15, CD30, CD34, EMA, and cytokeratin
HMB-45(-), ALK-1(-), HHV8(-)
Lymphocytes and plasma cells
T cells are usually more abundant than B cells
B cells and plasma cells are polytypic
In Situ Hybridization
Epstein-Barr virus encoded RNA (EBER)(+) in spindle cells in 40% of cases
Surrounding spleen is EBER(-) or degree of positive cells is significantly lower
Molecular Genetics
No evidence of monoclonal immunoglobulin or T-cell receptor gene rearrangements
EBV, when present, is monoclonal
Only a few cases have been studied
No known oncogene abnormalities
DIFFERENTIAL DIAGNOSIS
Splenic Inflammatory Pseudotumor (IPT)
Patients can be asymptomatic or present with mild systemic symptoms
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree