17 Infective endocarditis
Salient features
History
• Fever, malaise, anorexia, weight loss, rigors: non-specific symptoms of inflammation
• Progressive heart failure: caused by valve destruction (can be dramatic)
• Stroke, pulseless limb, renal infarct, pulmonary infarct: caused by embolization of vegetations
• Arthralgia, loin pain: caused by immune-complex deposition
• Obtain a history of recent dental procedures
• History of valvular heart disease, history of IV drug abuse
Examination
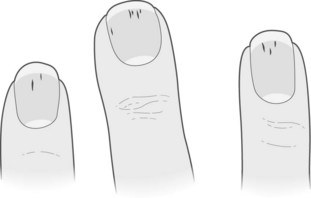
• Look for the following signs:
• Listen to the heart for murmurs and look for signs of cardiac failure.
• Examine the fundus for Roth’s spots (vasculitic phenomena).
• Examine the abdomen for splenomegaly.
• Look for embolic phenomena: stroke, viscera or occlusion of peripheral arteries.
• Test urine for microscopic haematuria (vasculitic phenomena).
• Remember that ostium secundum atrial septal defects almost never have infective endocarditis.
Questions
How would you investigate such a patient?
• Test the urine for microscopic haematuria.
• Take a FBC to show normocytic, normochromic anaemia and raised white cell count.
• Test for raised erythrocyte sedimentation rate (ESR).
• Blood culture: take three samples from different sites in 24 h. It is the most important test for diagnosing endocarditis and cultures are negative in >50% of cases of fungal aetiology.
• Transthoracic echocardiography may show vegetations. A negative study does not rule out endocarditis as vegetations <3–4 mm in size cannot be detected. Furthermore, all the leaflets of the aortic, tricuspid and pulmonary valves may not be visualized in every patient. Transoesophageal echocardiography is usually indicated in infective endocarditis.
What are the major categories of infective endocarditis?
Infective endocarditis can be classified as:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree