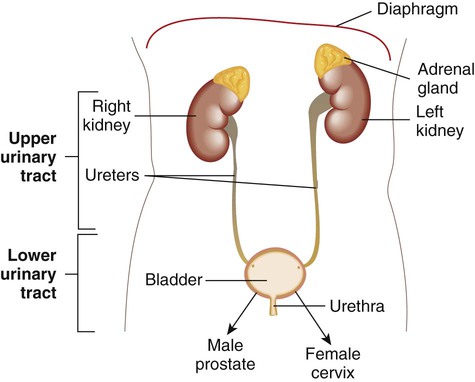
1. Describe the anatomy and identify the structures of the urinary tract, for both males and females. 2. Name the organisms that colonize the urethra and are considered normal flora. 3. Explain how the female urinary tract anatomy may predispose women to urinary tract infections. 4. Differentiate between community-acquired urinary tract infections and hospital-acquired urinary tract infections. 5. List the routes of transmission that allow bacteria to invade and cause a urinary tract infection. 6. Name the physical and chemical properties of urine that contribute to its role in the body’s defense mechanism against the bacteria capable of causing urinary tract infections. 7. Explain host and microbial factors that determine whether bacteria will be able to colonize and cause a urinary tract infection. 8. Name the properties bacteria possess that predispose them to having greater pathogenicity in causing urinary tract infections. 9. Define the five major types of urinary tract infections: pyelonephritis, cystitis, urethritis, acute urethral syndrome, and asymptomatic bacteriuria. 10. Compare and contrast complicated and uncomplicated urinary tract infections. 11. Explain the collection methods for urine specimens, including clean catch midstream urine, straight catheterized urine, a suprapubic bladder aspiration, and an indwelling catheter collection. 12. Describe the urine-screening methods available to determine bacteriuria and pyuria. 13. Explain the nitrate reductase test, the leukocyte esterase test, and the catalase test in regard to their urine-screening capability. 14. Name the media required for urine cultures. 15. Explain the proper methodology for plating and interpreting a quantitative urine culture. 16. Correlate signs and symptoms with the results of laboratory diagnositc procedures for the identification of the etilogic agent associated with infections of the urinary tract. The urinary tract consists of the kidneys, ureters, bladder, and urethra (Figure 73-1). The function of the urinary tract is to make and process urine. Urine is an ultrafiltrate of blood that consists mostly of water but also contains nitrogenous wastes, sodium, potassium, chloride, and other analytes. Urine is normally a sterile fluid, Often, urinary tract infections (UTIs) are characterized as being either upper (U-UTI) or lower (L-UTI) based primarily on the anatomic location of the infection: the lower urinary tract encompasses the bladder and urethra, and the upper urinary tract encompasses the ureters and kidneys. Upper urinary tract infections affect the ureters (ureteritis) or the renal parenchyma (pyelonephritis). Lower urinary tract infections may affect the urethra (urethritis), the bladder (cystitis), or the prostate in males (prostatitis). The urethra has resident microflora that colonize its epithelium in the distal portion; these organisms are lactobacilli, corynebacteria, and coagulase-negative staphylococci (Box 73-1). Potential pathogens, including gram-negative aerobic bacilli (primarily Enterobacteriaceae) and occasional yeasts, are also present as transient colonizers. All areas of the urinary tract above the urethra in a healthy human are sterile. Urine is typically sterile, but noninvasive methods for collecting urine must rely on a specimen that has passed through a contaminated milieu. Therefore, quantitative cultures for the diagnosis of UTIs have been used to discriminate among contamination, colonization, and infection. Activation of the host immune response by uropathogens also plays a key role in fending off infection. For example, bacterial contact with urothelial cells initiates an immune response via a variety of signaling pathways. Bacterial lipopolysaccharide (LPS; see Chapter 2) activates host cells to ultimately release cytokines such as tumor necrosis factor and interferon-gamma. In addition, bacteria can activate the complement cascade, leading to the production of biologically active components such as opsonins, as well as augment the host’s adaptive immune response. Host factors that lead to host susceptibility or resistance to uropathogens have been identified. For example, a glycoprotein synthesized exclusively by epithelial cells in a specific anatomic location in the kidney, referred to as Tamm-Horsfall protein or uromodulin, serves as an anti-adherence factor by binding to E. coli–expressing type 1 fimbriae (discussed later). Defensins, a group of small antimicrobial peptides, are produced by a variety of host cells such as macrophages, neutrophils, and cells in the urinary tract and attach to the bacterial cell, eventually causing its death. Although many microorganisms can cause UTIs, most cases are a result of infection by a few organisms. To illustrate, only a limited number of serogroups of E. coli cause a significant proportion of UTIs. Numerous investigations indicate that UPEC possesses virulence factors that enhance their ability to colonize and invade the urinary tract. Some of these virulence factors include increased adherence to vaginal and uroepithelial cells by bacterial surface structures (adhesins, in particular, pili), alpha-hemolysin production, and resistance to serum-killing activity (Box 73-2). Also, genome sequences of some UPEC strains have been determined, indicating that several potential virulence factor genes associated with the acquisition and development of UTIs are encoded on pathogenicity islands (e.g., hemolysins and E. coli P. fimbriae). Uropathogenic E. coli (UPEC) possess pathogenicity islands containing a variety of virulence factors. By definition, pathogenicity islands (see Chapter 3) contain genes that are associated with virulence and are absent from avirulent or less virulent strains of the same species. UTI encompasses a broad range of clinical entities that differ in terms of clinical presentation, degree of tissue invasion, epidemiologic setting, and requirements for antibiotic therapy. There are several types of UTIs: urethritis, ureteritis, asymptomatic bacteriuria, cystitis, the urethral syndrome, and pyelonephritis. Sometimes UTIs are classified as uncomplicated or complicated. Uncomplicated infections occur primarily in otherwise healthy females and occasionally in male infants and adolescent and adult males. Most uncomplicated infections respond readily to antibiotic agents to which the etiologic agent is susceptible. Complicated infections occur in both sexes. In general, individuals who develop complicated infections often have certain risk factors. Some of these risk factors are listed in Box 73-3. In general, complicated infections are more difficult to treat and have greater morbidity (e.g., kidney damage, bacteremia) and mortality compared with uncomplicated infections. Symptoms associated with urethritis (infection of the urethra), dysuria (painful or difficult urination), and frequency are similar to those associated with lower UTIs. Urethritis is a common infection. Because Chlamydia trachomatis, Neisseria gonorrhoeae, and Trichomonas vaginalis are common causes of urethritis and considered to be sexually transmitted, urethritis is discussed as a sexually transmitted disease in Chapter 74.
Infections of the Urinary Tract
General Considerations
Anatomy
Resident Microorganisms of the Urinary Tract
Infections of the Urinary Tract
Epidemiology
Pathogenesis
Routes of Infection
The Host-Parasite Relationship
Types of Infection and Their Clinical Manifestations
Urethritis
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Infections of the Urinary Tract