A. Altered stool consistency (diarrhoeal states)
1. Inflammatory bowel diseases
2. Infectious diarrhoea
3. Malabsorption syndromes
4. Short gut syndrome
5. Laxative abuse
6. Irritable bowel syndrome
B. Inadequate rectal reservoir or compliance
1. Inflammatory bowel disease
2. Radiation enteritis
3. Surgical resection of the reservoir:
(a) Low anterior resection of the rectum
(b) Ileoanal pouch surgery
4. Rectal ischaemia
5. Rectal neoplasia
6. Extrinsic rectal compression
7. Scleroderma and other collagen disorders
C. Altered rectal sensory function or motility
1. Cerebrovascular stroke
2. Central neurological trauma or neoplasia
3. Multiple sclerosis
4. Tabes dorsalis
5. Spina bifida
6. Myelomeningocele
7. Dementia
8. Peripheral neuropathy
9. Impaired motility and resulting overflow incontinence:
(a) Faecal impaction
(b) Anti-motility drugs
(c) Psychotropic drugs
10. Rectal hypermotility syndrome
D. Altered sphincter or pelvic floor mechanism
I. Anatomical or mechanical deficit:
1. Obstetric sphincter injury
2. Iatrogenic injury post anorectal surgery:
(a) Anal fistula surgery (lay open procedures)
(b) Haemorrhoidectomy
(c) Sphincterotomy
(d) Dilatation or anal stretch
3. Trauma
4. Neoplasia involving the sphincter
5. Congenital defects of the sphincter and pelvic floor:
(a) Imperforate anus
(b) Anal agenesis
II. Neurological deficit:
1. Neurogenic incontinence:
(a) Pudendal neuropathy
(b) Post vaginal delivery
2. Injury to spinal cord (cauda equina) or pelvic floor nerves (e.g. pelvic surgery)
3. Spina bifida and myelomeningocele
4. Diabetic neuropathy
III. Functional deficit:
1. Ageing
2. Sphincter atrophy
3. Prolonged rectal prolapse
4. Increased body mass index
Clinical Assessment
History Taking
Careful clinical history is extremely important. It is often required to tease out the complaints voiced by the patient and establish the presence of the problem in the first instance, as often patients do not verbalise their symptoms directly. In such circumstances, the distressing problem of incontinence might remain unaddressed or be mistreated, if the physician omits detailed clear history taking and enquiry.
The nature of the incontinence and whether it is predominantly an urge or passive leakage sheds light on the potential underlying pathophysiology. Passive incontinence, which is the involuntary loss of faecal matter or flatus to variable extent without conscious awareness, suggests a loss of perception and/or impaired rectoanal reflexes either with or without sphincter dysfunction [1]. Urge incontinence, which is the loss of faecal matter or flatus to variable extent in spite of an active attempt to retain them, suggests predominantly a disruption of the sphincter function or the rectal capacity to function as a reservoir [1]. Detailed history will also allow the differentiation of perineal soiling or mucus staining which can result from the presence of haemorrhoidal or rectal mucosal prolapse, fistula-in-ano or perineal sexually transmitted lesions. Enquiry about the ability to discriminate between formed or unformed stools and gas should be made. Moreover, it is important to delineate any symptoms of difficulty in evacuation or pelvic organ prolapse.
History of any precipitating factors, coexisting conditions such as diabetes mellitus or neurological conditions, past medical history, previous anorectal surgery, drug history and detailed obstetric history in female patients are also of great importance. An essential part of the history taking is establishing the extent of disruption and affliction on the patient’s quality of life and the ability to pursue their daily activities and their degree of willingness to undergo an invasive intervention to address the problem. This will help direct treatment strategies which are primarily aimed at improving patients’ quality of life and coping mechanisms.
Symptom Scores and Diaries
Validated incontinence scoring systems are an integral part of clinical assessment. Coupled with the use of prospective symptom diaries which supplement the snap shot questionnaire assessment by giving a record of clinical condition over the period of a week or more, they aid diagnosis, assessment of severity of symptoms and also help with monitoring the response to any treatment offered. A number of grading questionnaires have been designed aiming at quantifying the extent of symptoms into a numeric analogue assessment [2–4].
Examination
General and perineal examination is essential to identify the diagnosis. General examination may reveal a clue as to aetiology, such as signs of a neurological or connective tissue disorder. Inspection of the perianal area may reveal the presence of skin excoriation from exposure to faecal matter, a patulous anus or perineal descent. Other abnormalities like haemorrhoidal or rectal mucosal prolapse may be also diagnosed. Perineal scarring and small or absent perineal body would suggest previous obstetric trauma. The perianal sensations and the anocutaneous reflex should be also checked as impaired sensations or absent reflex suggest neuronal injury.
Digital rectal examination enables the examiner to assess (a) the bulk of the sphincter, (b) the presence of palpable defects, (c) the tone of the sphincter, (d) the quality of the squeeze function, (e) the presence of any rectal masses or rectocele and (f) the observation of pelvic floor dyssynergia. Digital examination is also of value to detect faecal impaction which can be associated with overflow incontinence. If a patient is suspected of having a rectal prolapse, this needs to be further evaluated whilst the patient is straining in the seated position.
At this stage, it has to be distinguished whether the incontinence is secondary to diarrhoea and a change in bowel habit or independent of stool consistency. If there is evidence of a change in bowel habit or other warning symptoms or signs, endoscopy (and other tests accordingly) is indicated to rule out mucosal pathology or neoplasia. Discussion of such workup is not within the merits of this chapter. Table 11.2 summarises the main components of clinical assessment.
Table 11.2
Clinical assessment in faecal incontinence
History | |
Personal history | |
Onset, course and duration | |
Nature of incontinence | Urge (sphincter or reservoir dysfunction) |
Passive (sensory dysfunction/internal sphincter dysfunction) | |
Mixed | |
Ability to distinguish solid, liquid and flatus | |
Prolapse symptoms | (Haemorrhoidal prolapse, rectal prolapse, global pelvic floor failure) |
Frequency of bowel motions | (Very infrequent motions might suggest overflow) |
Consistency of stools | (Diarrhoeal conditions and inflammatory bowel disease) |
Difficulty in rectal evacuation | (Dyssynergia, global pelvic floor failure, neurological conditions) |
Other bowel symptoms e.g. change in bowel habit, PR bleeding or tenesmus | (Investigate for mucosal pathology or neoplasia) |
Past medical history | Diabetes mellitus |
Neurological conditions | |
History of previous surgery | (Incontinence related to previous anorectal surgery which damaged the sphincter) |
Obstetric history | Number of pregnancies and deliveries |
Use of forceps | |
Previous tears | |
Drug history | |
Extent of interference with quality of life | |
Examination | |
General and back examination | (Signs of neurological disease or connective tissue disorder) |
Inspection of the perianal area | Skin excoriation from faecal matter |
Haemorrhoidal Prolapse | |
Scarring (Previous obstetric injury or anal surgery) | |
Small or absent perineal body (Previous obstetric injury) | |
Test anocutaneous reflex (stroking the perianal skin with a cotton bud leads to a brisk contraction of the external sphincter) | (Loss of the reflex suggests neuronal injury. Afferents are sensory nerves to the skin. Centre is spinal segments S2, 3, 4. Efferents are motor supply to external sphincter) |
Digital rectal examination | Is there faecal impaction |
Assess the bulk of the sphincter | |
Assess the presence of any palpable defects | |
Assess the tone of the sphincter | |
Assess the squeeze of the sphincter | |
Check for rectocele | |
Assess for dyssynergia of the pelvic floor | |
Check for rectal prolapse if suspected (straining in the seated position) |
Physiological Studies
Several physiological tests which often complement each other are available to assess anorectal functions. Physiological tests provide an objective assessment of anal sphincter pressures, rectoanal reflexes, anorectal sensory function and rectal compliance.
Anal Manometry
Standard Anal Manometry
Technique and Measurements
The equipment required for this test consists of four components: a probe, a pressure recording device, record-displaying device and a data storage facility (Fig. 11.1). Two types of probes are used: a solid-state probe with strain gauge transducers and a water-perfused probe. Technique details and equipment configurations significantly vary and examples have been published by various groups [5, 6]. Manometry is used to assess the resting and squeeze anal pressures, the cough reflex and the rectoanal inhibitory reflex (RAIR) (Fig. 11.2). Rectoanal pressure changes during simulated defecation can be also assessed in certain cases.

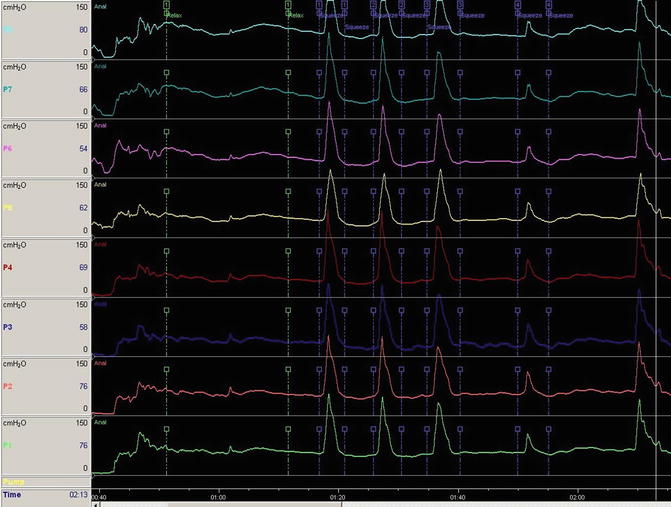

Fig. 11.1
Manometry stack
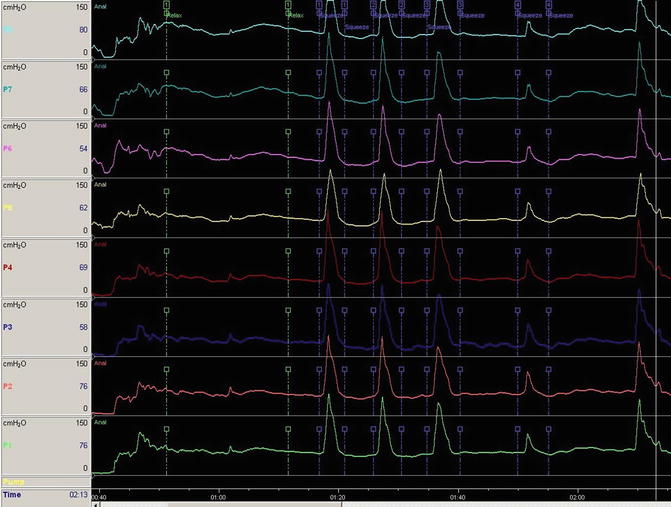
Fig. 11.2
Eight channel manometry trace (RAIR is not viewed on this trace)
Bowel preparation is not usually required but if digital rectal examination reveals faecal loading a preparatory rectal enema should be given. The patient is placed in the left lateral position with 90° flexion at the hips and knees. The procedure is preceded by digital rectal examination and the lubricated manometry probe is then gently inserted into the rectum. After a brief rest period to allow the sphincter tone to return to basal levels, measurements are taken during station pull through; the probe is gradually withdrawn in 0.5 or 1 cm steps and the recordings are taken when the transducer is stationery to avoid artefacts induced by reflex sphincter contraction during a rapid pull through procedure.
Resting anal pressure is defined as the difference between the intrarectal pressure and the maximum anal pressure at rest [5]. Pressures should be measured by averaging all four quadrants to account for sphincter asymmetry. Squeeze pressure is obtained by asking the patient to contract the sphincter for at least 30 seconds and to average the pressure measurement over this period [5]. The time interval in seconds during which the subject can maintain a squeeze pressure at or above 50 % of the maximum squeeze pressure represents the duration of sustained squeeze. The reflex increase in anal pressure during abrupt change in intra-abdominal pressure is tested by asking the patient to cough (cough reflex test) [7]. This protective reflex is thought to be mediated through a spinal reflex arc.
Clinical Utility
Studies have demonstrated high reproducibility of anal pressure measurements in the same subject on separate days [6]. Anal pressures are influenced by age and gender [7–9]; men have higher mean resting and squeeze pressures [10, 11] and pressures decline after the age of 60 years [10, 12]. There is relative lack of age- and sex-stratified normative data, and it is suggested that individual centres establish their own [5, 8]. Moreover, consideration of the different methods used to obtain the pressure measurements is essential when comparing the results of different studies.
The resting anal pressure predominantly represents the internal anal sphincter function and the voluntary squeeze pressure predominantly represents the external sphincter function. Normally, the high pressure zone which is the part of the anal canal where the resting pressure is >50 % of the maximum resting pressure is longer in males than females [13, 14]. In a normal individual the rise in pressure on maximal squeeze should be at least 50–100 % of the resting pressure [15].
Anal pressures are usually reduced in faecal incontinence [16–18]; however, in cases where aetiology does not involve sphincter malfunction (e.g. diarrhoea, disturbances of rectal sensations or compliance), anal pressures can be within normal range. Moreover, in a significant proportion of asymptomatic normal individuals, pressures were found to be low [19].
Differential reduction in anal pressures could reflect the site of deficit; a relatively maintained squeeze pressure with low resting pressure reflects a deficit in IAS function and vice versa. Reduced resting pressure is associated with passive leakage, whilst reduced squeeze pressure is associated with inability to delay rectal evacuation [20]. The loss of the normal cough reflex together with the voluntary squeeze function denotes a cauda equina lesion or a lesion in the sacral plexus, whereas in patients with spinal cord lesions above the conus medullaris, this reflex is present but the voluntary squeeze may be absent [21, 22].
Treatment of faecal incontinence cannot be monitored by changes in anal pressures. In some studies, anal pressures increased after biofeedback therapy; however, the magnitude of change was small and did not correlate with symptom improvement [23]. Similarly, changes in anal pressures following successful treatment with sacral nerve stimulation have been inconsistent [24].
Other Manometric Techniques
Ambulatory Manometry
This involves the use of micromanometers mounted on a catheter to simultaneously record rectal and anal canal pressures in a continuous manner [25, 26]. Although it provides information on the functioning sphincter in a more physiological situation in comparison with the static manometry, its use is primarily employed in the research setting.
Vector Volume Manometry (Vectometry)
This technique utilises a special device to automatically withdraw an eight-channel manometry catheter from the anal canal during rest and squeeze; and with the use of computer software, a three-dimensional reconstruction of the anal canal is then produced [27]. Vectrometry can be used to differentiate between global sphincter atrophy or weakness and traumatic sphincter injury by demonstrating global weakness or significant asymmetry indicating a localised sphincter abnormality respectively [27, 28]. However, poor correlation between the asymmetry on the vectogram and the electromyographic or ultrasound localisation of sphincter defects was demonstrated in some studies [29] and endoanal ultrasound remains the gold standard for identifying anal sphincter defects [30]. Nevertheless, a recent review suggests that vectrometry results correlate well with imaging and that clinical utility can be improved with the standardisation of technique and equipment [31].
High-Resolution Anorectal Manometry
This new approach utilises high-resolution techniques in combination with novel rapid data-interpretation software to allow the interpolation of manometric recordings into highly detailed topographical plots of the anorectal intraluminal pressure events relative to time [32]. Results of this technique seem to be well collaborated with conventional measurements and further studies are being conducted to establish its place in routine assessment.
Recto-Anal Inhibitory Reflex (RAIR)
Reflex relaxation of the upper internal anal sphincter (IAS) occurs with progressive rectal filling and is a physiological phenomenon vital to the continence mechanism. Representing the close association between anorectal sensations and motor function, this ‘sampling reflex’ occurs regularly allowing rectal contents to be presented to the specialised lower anal sensory mucosa where it can establish its nature (solids, fluid or gas) [33, 34]. The contents are delivered back to the rectum by the effect of the high pressure generated by the presence of the external anal sphincter (EAS) overlapping the lower anal canal [35]. Figure 11.3 demonstrates the various components of this reflex.
Fig. 11.3
The various components of the RAIR reflex on a manometry trace: (a) Excitation peak: initial increase in the resting pressure associated with the sudden rectal distension. (b) Latency (X–Y): duration from the point of excitation peak back to the baseline pressure. (c) Point of maximum relaxation (Z): lowest point of resting pressure secondary to reflex IAS relaxation. (d) Recovery time (Z–Z1): the duration between maximum relaxation and the point at which the resting pressure recovers to two thirds its baseline. (e) Total reflex duration (X–Z1): calculated as the duration from the point of the Excitation Peak to the point two thirds’ the recovery (Z1)
Technique and Measurement
The RAIR is recorded as part of the anorectal manometry study. This normal reflex is elicited by rapidly inflating a balloon in the rectum whilst simultaneously recording the anal pressure to demonstrate the IAS relaxation. Most currently available manometry catheters are manufactured with a mounted balloon to facilitate this test (Fig. 11.4).


Fig. 11.4
Eight channel manometry catheter with a balloon
Clinical Utility
The RAIR was first described by Gowers in 1877 [36] and was later confirmed in 1935 by Denny-Brown and Robertson [37]. It is thought to be mediated via the intramural neuronal plexus [34], and its absence is used as a diagnostic criterion for Hirschsprung’s disease [38–40]. The reflex is also absent following rectal resections; however, there is some evidence that it recovers with time [41, 42]. Some studies have demonstrated specific changes to this reflex in association with disturbed continence. Kaur et al. showed significantly greater sphincter relaxation in the incontinent patients as compared with constipated patients or control subjects [43]. Others have shown that the volume required to induce the reflex was lower in incontinent patients than controls [18, 44].
Anal Sensory Testing
The anal canal mucosa has a plethora of afferent nerve endings allowing the perception of wide range of sensory modalities including touch, pain and temperature [45]. Intact anal sensory function is vital to the continence mechanism.
Technique
Intactness of anal sensory function is clinically tested using electric stimulation. A bipolar electrode and a signal generator are used to provide a wave impulse at 5 Hz of 100 μs duration. The electrode catheter is placed in the anal canal and the current is incrementally increased (up to a maximum of 20 mA) until the subject reports a tingling or pricking sensation. The lowest recorded current of three readings is noted as the sensory threshold [46].
Clinical Utility
Normal electrical sensory threshold in the anal canal is 4 mA (2–7 mA) [46, 47]. Thresholds increase with age and thickness of the subepithelial layer of the anal canal [47]. The primary role of testing for anal sensations in the context of assessment of faecal incontinence is in identifying hindgut (somatic) denervation which can be present in neurogenic incontinence (e.g. in spinal cord injury, multiple sclerosis and diabetic neuropathy) [21, 48–50].
Rectal Sensory Testing
Intact rectal sensory function is an integral component of the mechanism of continence. In contrast to the anal canal, the modalities of rectal sensations are indistinct (visceral sensations) and the rectum is insensitive to stimuli capable of producing pain and other sensations when applied to a somatic cutaneous surface [45, 51]. Full understanding of the types and functions of rectal receptors is still lacking [45, 52]. Rectal distension is associated with the perception of rectal filling and the coordination of specific anorectal reflexes, and although the nature of the mediating receptors is not fully delineated, specialised mechanoreceptors are most probably responsible [52]. Intraganglionic Laminar Endings (IGLEs) are known to be present in the upper gastrointestinal tract; however, recent animal work has revealed that the rectum contains morphologically and functionally unique IGLEs [53]. In clinical practice, testing rectal sensations is performed by two ways (mucosal electrosensitivity and balloon distension). A recent study showed good reproducibility of a newly designed multimodal rectal probe used to test electrical, thermal and mechanical sensory modalities in the rectum [54].
Electric Sensory Thresholds
Technique
This is assessed using a bipolar electrode catheter and pulse generator similar to those used for anal sensory testing. However, the stimulus used is modified to the frequency of 10 Hz and the duration of 500 μs. The threshold is determined by gradually increasing the stimulus (up to a maximum of 50 mA) until the subject reports perception of lower abdominal discomfort or colicky sensation [46, 55].
Clinical Utility
Normal electric sensory thresholds in the rectum range widely between 2.9 and 53.0 mA and is usually higher in females in comparison with males [56]. Patients with neurogenic incontinence have impaired sensation to electrical stimulation [49]. In a study of 68 subjects, Meagher et al. demonstrated circumferential variation of rectal electric sensory threshold suggesting that it is the pelvic floor rather than rectal mucosa which is stimulated with this testing modality [57].
Balloon Distension Thresholds
Technique
Rectal distension thresholds can be tested either by manually distending a latex rectal balloon or by distending a polyethylene rectal balloon using a barostat device [30, 55]. The use of the barostat permits more controlled distensions and therefore provides more physiological and less rater-dependent assessment. Moreover, it enables the measurement of changes in both pressure and volume on distension, therefore permitting assessment of pressure-volume relationships and rectal compliance [58].
The distension thresholds assessed clinically include [7, 9, 59–61] (a) first sensation (FS) (first awareness of the intrarectal balloon), (b) desire to defecate (DD), (c) urgency to defecate (U) and (d) maximally tolerated volume (MTV) (the volume which can be tolerated in total before pain occurs).
Clinical Utility
Sensory thresholds to rectal distension in asymptomatic subjects vary significantly between different centres [7, 9, 59–61]. The pattern of balloon distension [62] as well as age of the subject [9] affects rectal perception. The large inter- and intra-subject variation in values and the wide normal range impact the clinical value of these measurements [63]. Moreover, thresholds for rectal distension may be elevated, normal or reduced in faecal incontinence [16, 17]. Nevertheless, evidence of loss or significant reduction of rectal perception to balloon distension (hindgut denervation) and conversely the evidence of exaggerated rectal sensation (rectal hypersensitivity and/or reduced rectal capacity) are important findings when assessing faecal incontinence. Impaired rectal sensation can be associated with symptoms of incontinence [64, 65], and there is evidence that sensory retraining can improve symptoms [65, 66]. On another hand, some patients with urge faecal incontinence have significantly reduced sensory thresholds to rectal distension; this rectal hypersensitivity has been found to be associated with reduced rectal compliance and exaggerated rectosigmoid motor activity highlighting a specific entity of incontinent patients [17, 67].
Rectal Compliance Measurement
Given a slow filling rate, the intraluminal rectal pressure does not increase until the maximum tolerated volume is approached; this phenomenon of receptive relaxation (compliance) of the rectal wall defines the rectum as a reservoir.
Technique
Rectal compliance is measured by assessing rectal pressure-volume relationships, either by manually inflating a latex balloon inside the rectum with air or water or by mechanically distending an infinitely compliant bag using the barostat device. The latter is the preferable technique as it utilises a controlled rate of distension and an infinitely compliant bag, eliminating technical sources of variability [6, 58, 68]. The polyethylene barostat bag has to be infinitely compliant, either a bag infinitely compliant up to its maximum volume or a fixed large-volume noncompliant bag which has a maximum volume greater than the maximum volume of the rectum [69]. Mechanical instillation of air into the bag by the barostat device allows for the standardisation of flow rate and accurate measurements of volume-pressure relationship. Specific sequence of distension protocols is used and the pressure-volume data obtained is plotted on special software to calculate compliance (change in volume divided by change in pressure).
Clinical Utility
Rectal compliance is a measure of the combined sensorimotor function of the rectum. Barostat measurement of rectal compliance using identical distension protocols has been shown to have good inter- and intra-subject reproducibility [6, 58, 68]. Abnormal compliance has been demonstrated in patients with various anorectal dysfunction, but interpretation of results can be problematic due to the lack of standardised protocols for measurement and the contribution of abnormal rectal sensations [52]. Normal rectal compliance is 11.9 ± 4.1 mL/mmHg [58]. Rectal compliance is reduced in patients with colitis [70] and in some patients with systemic sclerosis [71, 72].
Symptoms of faecal urgency and urge incontinence may be associated with reduced compliance and rectal capacity [17, 67, 73], however, changes in compliance may be secondary to the incontinence and not causative [73]. Moreover, the contributory factor of changes in the rectal sensory function makes interpretation difficult. Some studies have suggested that reduced compliance is associated with reduced rectal sensitivity [74, 75]. Nevertheless, other studies in healthy subjects [76], patients following radiotherapy [77] and ulcerative proctitis [70] suggest that reduced rectal compliance is associated with and perhaps contributes to rectal hypersensitivity.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


