Fig. 3.1
Endoanal ultrasound demonstrating normal sphincter anatomy. Subepithelium (dotted arrow) and internal anal sphincter (thin arrow). The longitudinal muscle (square) and external anal sphincter (circle) with comparable reflectivity are distinguished by their interface reflections
The subepithelium forms the innermost layer. It is mildly hyperreflective (i.e. “bright”) and contains the muscularis submucosae ani and vascular channels. The IAS forms the innermost muscular layer and extends from the anorectal junction to approximately 1–1.5 cm below the dentate line. Its characteristic features are of a low-reflectivity (i.e. dark), very well-demarcated ring. As discussed below, the thickness of internal sphincter when measured by ultrasound varies according to age, but it is usually symmetric in the mid canal, although may appear thinner anteriorly, particularly in the upper canal in females. Significant asymmetry in the internal sphincter suggests either focal atrophy or injury (Fig. 3.2). One caveat to this rule however is in the distal canal—an asymmetric termination of the internal sphincter is relatively common in normal individuals which may give the impression of a distal defect to the inexperienced. Conventionally the internal sphincter is measured at its thickest portion at either 3 or 9 o’clock.
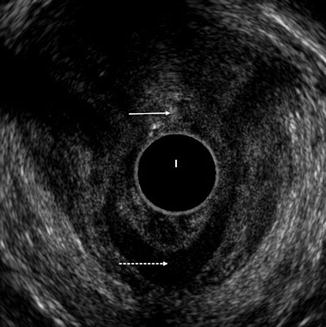
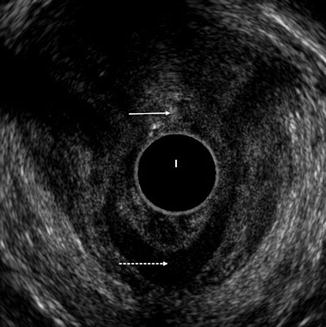
Fig. 3.2
Endoanal ultrasound with an anterior tear of the internal and external anal sphincters (thin arrow). Note the retraction of the internal anal sphincter posteriorly (dotted arrow)
The longitudinal muscle interdigitates between the EAS and IAS and terminates in the subcutaneous EAS and subcutaneous peri-anal soft tissues. Sub-adventitial fat on either side of this layer creates interface reflections (“bright lines”); the outer reflection between the longitudinal layer and the external sphincter borders the intersphincteric space. It is postulated that the longitudinal layer functions to brace the anus preventing eversion during defaecation [4]. The ability to clearly depict the longitudinal muscle with ultrasound differs between individual patients but when seen is usually hyporeflective (darker) in comparison to the surrounding echogenic (bright) fat.
The EAS is anatomically composed of three cylindrical bundles. The EAS forms the outermost muscle of the anal canal and extends distally approximately 1 cm beyond the IAS. The deep part is fused to the puborectalis muscle. The EAS is anteriorly related to several identifiable structures including the superficial transverse muscle of the perineum and the perineal body. The transverse perineal muscles usually merge with the anterior EAS in women, but a clear plane is commonly seen between the two in men. Posteriorly the EAS is continuous with the anococcygeal ligament, the low reflectivity of which can sometimes be mistakenly confused for a posterior sphincter defect. Importantly, as discussed below, the EAS is much shorter in women than men [5], and again the inexperienced may confuse this anatomical difference with a sphincter defect. The outer border of the external sphincter is demarcated by the interface reflection with fat in the ischioanal fossa. In cases of fatty atrophy of the external sphincter, this outer border may be difficult to confidently discern on ultrasound, and as discussed below, MRI is superior in assessing EAS atrophy and muscle quality. Indeed, there is good data showing greater interobserver variation in EAS thickness measurement compared to the better-visualised IAS: Gold et al. [6] reported that the 95 % limits of agreement for EAS measurements span 5 mm, compared to just 1.5 mm for the IAS.
As the examination commences in the proximal anal canal, the puborectalis and transverse perineal muscles should be identified. The puborectalis can be distinguished from the EAS as it slings around the anorectal junction and has anterior ends that splay outwards as they point to their insertion at the pubic arch. Once the probe is withdrawn a couple of centimetres, the puborectalis will blend imperceptibly with the EAS and where the sphincter forms a complete ring anteriorly demarcates the mid anal canal. The IAS is also thickest and imaged best at this location. Further withdrawal of the probe images the subcutaneous EAS, and at this level the IAS has usually terminated.
Anatomical Variations
There is clear anatomical variation between men and women in anal canal anatomy [5]. The external sphincter is generally shorter in women, particularly anteriorly. Using 3D ultrasound, Williams et al. reported that on average the external sphincter was approximately 17 mm long in women compared to 30 mm in men. The external sphincter is also usually less reflective in men compared to women and therefore easier to visualise. Conversely, little gender differences have been found in the length of either the puborectalis or the IAS.
Sphincter thickness as depicted by endoanal ultrasound is not constant throughout life; notably IAS thickness increases with age. Measurements of 1–2 mm for young adults, 2–3 mm for middle-aged adults and 3–4 mm for the elderly are typical (Fig. 3.3). As the sphincter becomes thicker with age, a small increase in reflectivity may also be noted, attributable by some to a more prominent connective tissue component [7]. Conversely, the external sphincter tends to thin in older nulliparous women, whereas the subepithelium and longitudinal layer tend to remain unchanged [7].
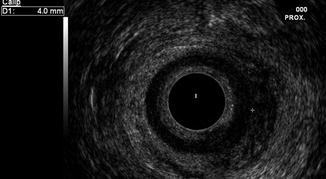
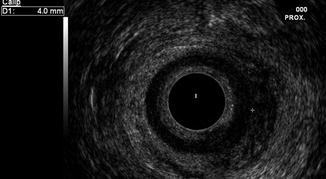
Fig. 3.3
Endoanal ultrasound demonstrating thickened internal anal sphincter (4 mm) in a 50 year old woman (see calipers)
MRI
Basic Technique
In general MRI examination of the anal canal is more complex than endoanal ultrasound. Image quality, for example, can be improved by patient preparation such as a period of fasting to reduce peristalsis artefact, and an empty bladder is preferred.
There are two main approaches to performing anal canal MRI; either the MRI coil is placed over the pelvis of the patient (i.e. externally) or a specially designed endocavity coil is inserted into the anal canal, similar to an endoanal ultrasound probe, although usually of marginally greater diameter. The endoanal coil is introduced with the patient in the left lateral decubitus position, and a supine position is then adopted with the coil secured with cushioning sandbags prior to imaging [8].
Although use of an endocoil is clearly a much more invasive approach impacting on patient acceptability, acquired images have a higher spatial resolution than those produced using an external pelvic coil alone, and highly detailed images can be obtained. However, the field of view (volume of tissue imaged) using an endocoil is restricted—only the anal sphincter complex and a few centimetres of surrounding tissue are well visualised. Conversely the field of view is much greater using an external coil where not only the anal canal is interrogated (albeit with slightly lower but usually adequate spatial resolution) but also the surrounding tissues of the pelvis. Such greater anatomical coverage assumes importance when imaging pathological conditions which often stray beyond the confines of the anal sphincter complex such as peri-anal sepsis and anal cancer. Although many of the early descriptions of anal canal MRI anatomy were based on studies using an endocoil, in clinical practice imaging using the external pelvic coil is overwhelmingly now the preferred option, and the use of endocoils is restricted to a handful of specialist centres.
While there is some debate as to the optimal MR sequence combinations used to image the anal canal, in reality several sequences are useful and choice boils down to the target pathology and individual radiologist preference. T1-weighted IV contrast-enhanced MR imaging, short-inversion-time inversion recovery (STIR) imaging and T2-weighted spin-echo MR imaging are all advocated [9–11] (Table 3.1). A basic T2-weighted fast spin-echo is generally recommended when precise depiction of anal canal anatomy is required since it optimises contrast between the low-signal anal sphincters and the surrounding high-signal fat (see Table 3.1) [12]. Conversely, sequences which null the signal from fat (either fat-saturated T2 or STIR) are particularly useful in depicting peri-anal sepsis when it is important to highlight fluid in tracts, which appear as “bright” high signal. Perhaps the key to successful MRI of the anal canal is optimal slice orientation. It is vital to acquire images carefully aligned to the plane of the anal canal; otherwise, the anatomy is distorted and interpretation much more difficult. Straight axial images through the pelvis are particularly problematic since the anal canal axis is approximately 45° to this. It is paramount therefore to have well-trained radiographic staff supervise the acquisition of anal MRI.
Table 3.1




T2-weighted fast spin-echo sequence recommendations [12]
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


