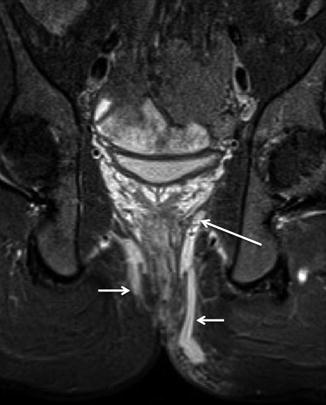
Fig. 18.1
Anal endosonography of a man with a transsphincteric fistula (same patient as Fig. 18.4). There is a hyporeflective track (arrows) through the external sphincter, but it is more difficult to appreciate that this is due to a transsphincteric fistula than on the corresponding MR image unless the sonographer is very experienced
MRI Technique
Over the last decade, MRI has emerged as the leading contender for preoperative classification of fistula-in-ano. This is because MRI can vividly separate infected tracks and extensions from surrounding structures, imaging both with precision. Furthermore, MRI can image in the surgically relevant coronal plane so that the geographical course of the fistula can be determined. Indeed, the ability of MRI to not only accurately classify tracks but also to identify disease that would otherwise have been missed has had a palpable effect on surgical treatment and, ultimately, patient outcome [7, 8].
Field strength does not appear to be a critical factor, and excellent results can be obtained using relatively modest MRI scanners with no need for specialised coils. External phased array surface coils increase signal-to-noise ratio (SNR) and spatial resolution, to good effect [9, 10], and are generally available. Although the best spatial resolution is achieved by using dedicated endoluminal anal coils [11], these suffer the same limitation as AES – the limited field of view means that distant extensions will be missed [12]. Because of this, they are now rarely used. It should also be stressed that anal endoluminal coils are not the same as rectal coils. Rather, they are smaller in diameter and are intended to cross the anus.
The MRI sequences used to image fistula-in-ano need to combine anatomic precision (so that the course of the fistula with respect to adjacent structures can be determined), with the facility to highlight sepsis (usually pus). Many investigators employ the rapid and convenient fast spin-echo T2-weighted sequence, which provides good contrast between hyperintense fluid within the track and its hypointense fibrous wall while simultaneously enabling good discrimination between the several layers of the anal sphincter. Fat suppression techniques are very useful. The earliest reports used STIR imaging, with the addition of T1-weighted scans to help anatomical clarification [13], and gadolinium contrast may be used if desired [14]. While other approaches have included saline instillation into the external opening or rectal contrast medium, such measures increase examination complexity in the face of the already excellent results achieved by less invasive procedures, and there is little motivation to adopt them. For the majority of their clinical work, the authors use a 1.5 T magnet and STIR sequences in just two planes, combined with the sagittal acquisition described below, which makes for a very rapid and easy examination.
It is central to success that imaging planes are correctly aligned with respect to the anal sphincter. Because the anal canal is tilted forward from the vertical by approximately 45°, straight axial and coronal images with respect to the patient/scanner tabletop will result in oblique images of the anus, and the geography of any fistula will be difficult to ascertain. This is especially so when trying to determine the height of the internal opening. Oblique axial and coronal planes orientated orthogonal and parallel to the anal sphincter are definitely necessary and are most easily planned from a midline sagittal image (Fig. 18.2). It may be necessary to align supplementary scans to the rectal axis in complex cases with an internal opening high in the rectum, but this is seldom necessary. It is important that the imaged volume extends several centimetres above the levator muscles and also includes the whole presacral space, both of which are common sites for extensions. The entire perineum should also be included. Occasionally, tracks may extend for several centimetres, even leaving the pelvis or reaching the legs, and any track visible on the standard image volume must be followed to its termination if this has not been included. The precise location of the primary track (e.g. ischioanal or intersphincteric) is usually most easily appreciated using axial images, and the radial site of the internal opening is also well seen using this plane. Coronal images best visualise the levator plate, which separates supra- from infralevator infection. The height of the internal opening may also be best appreciated on coronal images, with the caveat that the anal canal must be imaged along its entire craniocaudal extent, as explained above.
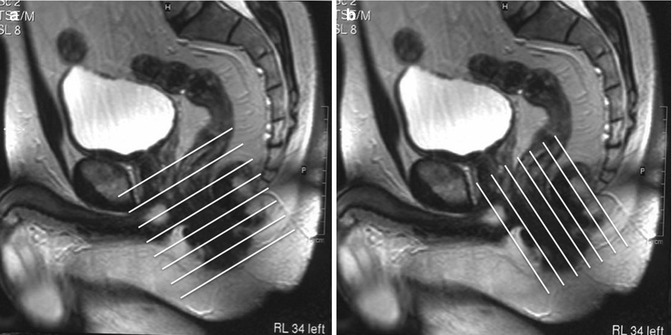
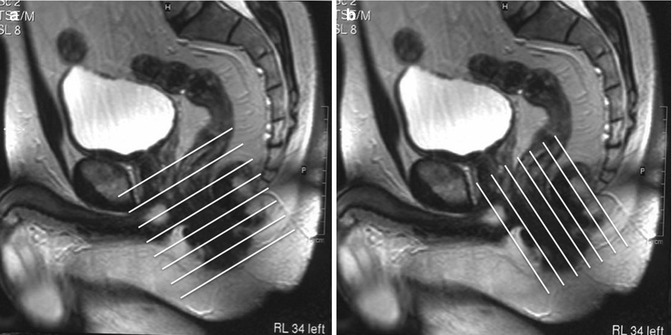
Fig. 18.2
Sagittal T2-weighted planning scan showing the orientation of the anal canal and the oblique axis to which the axial (a) and coronal (b) scans must be aligned (white lines). Images should extend well into the supralevator compartment and also cover the entire presacral space
MRI Interpretation
All competent MRI reports should include the following information: The radial location and classification of the primary track(s), the radial location and level of the internal opening(s) and a description of any extensions.
Active tracks are filled with pus and granulation tissue and thus appear as hyperintense on T2-weighted or STIR sequences, often surrounded by hypointense fibrous walls, which can be relatively thick, especially in patients with recurrent disease following previous surgery. The external anal sphincter is relatively hypointense, and its lateral border contrasts sharply against the fat within the ischioanal fossa, especially on T2-weighted studies. Consequently it is relatively easy to determine whether a fistula is contained by the external sphincter or has extended beyond it.
If a fistula remains contained by the external sphincter throughout its course, then it is highly likely to be intersphincteric (Fig. 18.3). In contrast, transsphincteric, suprasphincteric and extrasphincteric fistulas all show sepsis in the ischioanal space – it is the level of the internal opening and the level at which the fistula crosses the sphincter complex that differentiates between these types. A track in the ischioanal fossa is usually due to a transsphincteric fistula (Fig. 18.4) simply because it is much commoner than suprasphincteric or extrasphincteric classifications.
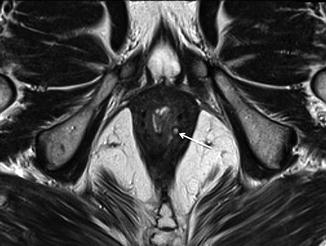
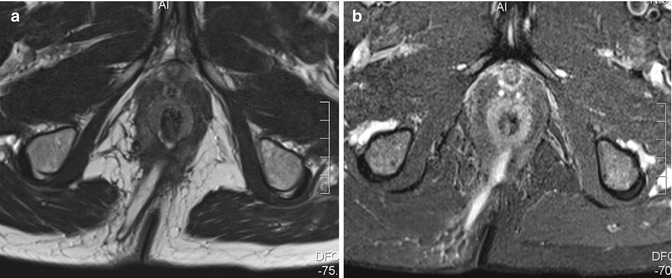
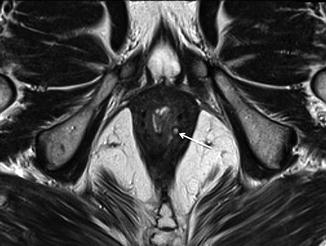
Fig. 18.3
Axial T2-weighted MR images in a man with an intersphincteric fistula (arrow). Note that the fistula is contained by the external sphincter; there is no sepsis in the ischioanal fossa
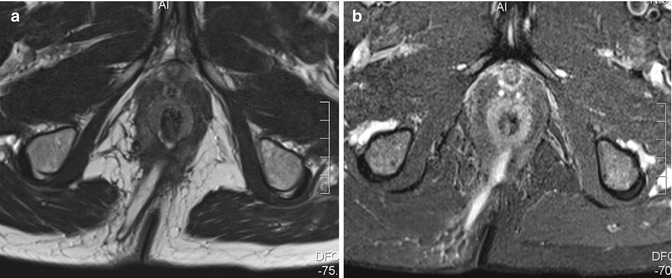
Fig. 18.4
Axial T2-weighted (a) and STIR (b) images in a man with a transsphincteric fistula in the right posterior quadrant with an internal opening at 6 o’clock at dentate line level (same patient as Fig. 18.1)
The exact location of the internal opening can be difficult to define. Two questions need to be answered: what is the radial site of the internal opening and what is its level? The vast majority of anal fistulas open into the anal canal at the level of the dentate line, commensurate with the cryptoglandular hypothesis of fistula pathogenesis. Furthermore, most fistulas also enter posteriorly, at 6 o’clock. Although the dentate line cannot be identified as a discrete anatomical entity, even when using endoanal receiver coils, its general position can be estimated with sufficient precision by an experienced radiologist. The dentate line lies at approximately mid-anal canal level, which is generally midway between the superior border of the puborectalis muscle and the most caudal extent of the subcutaneous external sphincter. These landmarks define the ‘surgical’ anal canal (as distinct from the ‘anatomical’ anal canal, which is shorter, and defined as the canal caudal to the anal valves). Dentate level is best estimated using coronal views, which allow the craniocaudal extent of the puborectalis muscle and external sphincter to be appreciated, but its location can also be estimated from axial views given sufficient experience. It should be noted that in many patients the puborectalis muscle is rather gracile, unlike the bulky muscle suggested in many anatomical illustrations. Notably, the puborectalis frequently blends imperceptibly into the external sphincter, which hampers precise identification of mid-anal canal level on imaging. Nevertheless, this can be overcome with experience. Any fistula track that penetrates the pelvic floor above the level of the puborectalis muscle is potentially a suprasphincteric or extrasphincteric fistula. The level of the internal opening distinguishes between these, being anal in the former (Fig. 18.5) and rectal in the latter (Fig. 18.6). Transsphincteric fistulas penetrate the external sphincter directly, a feature that can be easily appreciated on axial or coronal views (Fig. 18.4). However, recent MR studies have revealed that a transsphincteric track may cross the sphincter at a variety of angles [15]. For example, it may arch upwards as it passes through the external sphincter and thus cross the muscle at a higher level than would be deduced merely from inspecting the level of the internal opening. This is important because such tracks will require a greater degree of sphincter incision during fistulotomy, with a correspondingly increased risk of post-operative incontinence. Coronal MRI is best placed to estimate the precise angulation of the track with respect to the surrounding musculature [15].
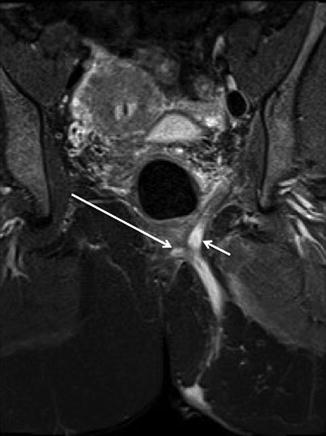
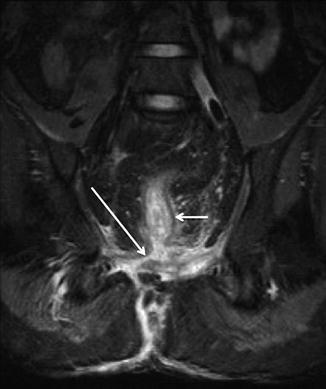
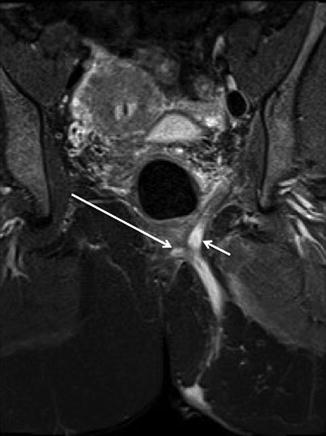
Fig. 18.5
Coronal STIR MRI in a patient with a suprasphincteric fistula. The primary track is arching over the puborectalis (long arrow). There is also a small cranial extension off the apex of the track (short arrow) into the roof of the left ischioanal fossa
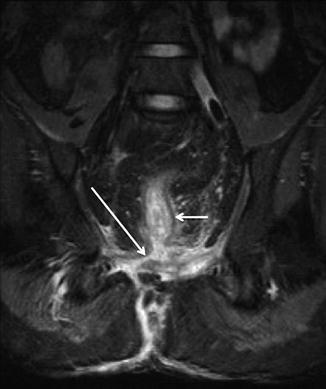
Fig. 18.6
Coronal STIR MRI in a man with an extrasphincteric fistula. Note that the primary fistula track has a rectal opening (long arrow) above the level of the levator plates (rectum = short arrow)
The radial site of the internal opening is simple to identify if the fistula track can be traced right to the anal mucosa, but this is unusual because the internal opening is rarely widely patent – rather it is most often compressed and can be very difficult to see. In many cases an intelligent deduction must be made as to where the internal opening is likely to be. This is best achieved by looking to where there is maximal intersphincteric sepsis, since the internal opening is likely to lie adjacent or very close to this. The intersphincteric space and longitudinal layer are often seen as a low intensity ring lying between the internal and external sphincter. The internal sphincter is hyperintense on both T2-weighted fast spin echo and STIR sequences.
Extensions
The major advantage of MRI is the ease with which it can image any extensions associated with the primary track. Like tracks, extensions are manifest as hyperintense regions on T2-weighted and STIR imaging and also enhance further if intravenous contrast is given. Again, collateral inflammation can be present to variable extent. The commonest type of extension is one that arises from the apex of a transsphincteric track and extends into the roof of the ischioanal fossa (Fig. 18.7).