Iatrogenic Changes
Key Facts
Etiology/Pathogenesis
Pathologic changes occur in breast due to prior surgery, radiation therapy, and medical treatment
Treatment-related changes are important to recognize
Clinical Issues
Excisions after core needle biopsy must document prior biopsy site
Biopsy site changes must be correlated with prior clinical history and treatment
Recurrent carcinomas should be distinguished from new primary carcinomas
Tumors caused by treatment should be recognized
Biopsy-associated fibromatosis
Radiation-associated sarcoma
Radiation-associated carcinoma
Implant-associated lymphoma
Fibroadenomas associated with cyclosporine
Carcinomas associated with hormone replacement therapy
Iatrogenic changes can mimic malignancy
Squamous metaplasia
Radiation atypia
Epithelial displacement
Degenerating skeletal muscle
Neuromas
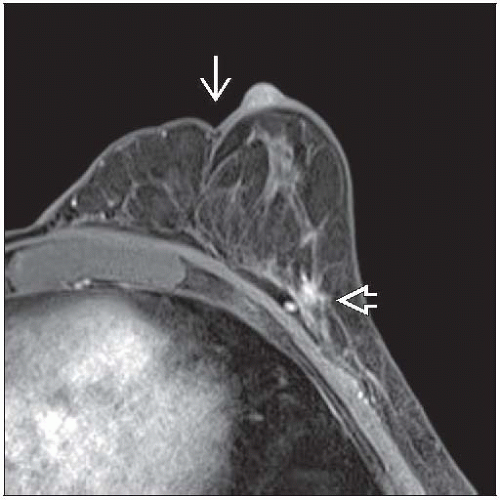
Image Findings
May be difficult to detect recurrent carcinoma
Top Differential Diagnoses
Ruptured cysts
Fat necrosis
Tumors mimicking inflammatory lesions
TERMINOLOGY
Definitions
Pathologic changes in breast due to prior treatment (surgery, radiation, or medical treatment)
ETIOLOGY/PATHOGENESIS
Treatment-related Changes
Breast is unusual organ in that entire organ is typically not removed and multiple surgical procedures are often performed over short period of time
Thus, recent biopsy sites and excisional sites as well as older excisional sites are common findings in breast specimens
Medical treatments and radiation therapy can also result in pathologic changes
Recognition of changes associated with prior treatment is important to understand relationship of breast lesions to these prior procedures and to avoid misinterpretation of iatrogenic changes as malignancy
Documentation of Removal of Targeted Lesion
Excisions after core needle biopsy must include prior biopsy site
Specimen radiography should document removal of any residual lesion &&/or clips marking site
In some cases, clip may not have been deployed at site of lesion
In other cases, clip may be lost if biopsy site is transected during procedure
Histologic findings of core biopsy site must be documented
However, if excision occurs > 1 month after biopsy, inflammatory changes may have resolved
Margin excisions should include a portion of prior biopsy cavity
Biopsy site changes at margin may indicate incomplete removal of a lesion
Indication of Important Clinical History
Results of any prior excision should be available
Interpretation of residual lesions may be altered with respect to prior history
If there is prior history of cancer, patient may have received treatment
Radiation therapy can cause nuclear atypia
These changes could be mistaken for neoplasia if pathologist is unaware of this history
Recurrence vs. New Primary Invasive Cancers
Recurrent invasive cancers have poor prognosis as they are treatment resistant
These cancers usually occur at site of original cancer
New primary carcinomas have a better prognosis as they may be sensitive to treatment
Prior biopsy sites can sometimes be recognized by dense fibrosis &&/or suture material
If present, it is important to document location of 2nd carcinoma with respect to 1st
Treatment-associated Tumors
Some types of treatment can cause tumors
Fibromatosis associated with surgery (or breast implant)
May occur at site of prior surgery
Radiation-associated sarcoma
Most commonly, angiosarcoma of skin after radiation therapy for breast carcinoma
Radiation-associated carcinoma
Occurs in women undergoing radiation to breasts during late teens and early 20s
Radiation at later ages does not markedly increase cancer risk
Implant-associated lymphoma
Very rare form of T-cell lymphoma has been reported in ˜ 30 cases of women with breast implants
Lymphoma is found in a seroma cavity surrounding implant
Cyclosporine-associated fibroadenomas
Renal transplant patients treated with cyclosporine may develop fibroadenomas
Fibroadenomas can regress when cyclosporine is withdrawn
Hormone replacement treatment-related carcinomas
Women taking hormonal therapy after menopause are at increased risk for estrogen receptor-positive cancers
It is unknown if estrogen acts as a carcinogen to cause cancers or if it stimulates growth (and therefore detection) of already existing carcinomas
IMAGE FINDINGS
Mammographic Findings
Prior surgical sites generally have an irregular appearance
May be difficult to detect recurrent carcinoma
Radiodense debris can be present due to surgical procedure (e.g., metallic fragments)
Associated fat necrosis can calcify
For excisional sites, skin scar will be present
MACROSCOPIC FEATURES
Core Needle Biopsy Sites
Site usually has small central area of hemorrhage (˜ 0.5 cm) surrounded by ill-defined area of firm tissue and fat necrosis
Clip is very small (1-2 mm) but may be seen with careful examination
Some clip deployment systems place gelatin foam pledgets within biopsy site
These are often color and shape of rice
May be mistaken for calcifications or papilloma
Usually fall out of tissue
Some systems use larger rectangular-shaped gel
May be surrounded by pseudocapsule with minimal inflammatory response
If gel falls out of tissue, site can be difficult to identify
If core biopsy was of small invasive carcinoma, size of carcinoma may be difficult to ascertain grossly
Correlation with imaging studies prior to biopsy may be necessary to determine best size for AJCC T classification
Excisional Sites
There is generally bleeding at center of excisional site and loss of tissue
Surrounding tissue is firm but not hard and may extend for several millimeters into surrounding breast
Fat necrosis appears as chalky white or yellowish streaks
Residual invasive cancer may be present as areas hard to palpation adjacent to cavity
MICROSCOPIC PATHOLOGY
Core Needle Biopsy Sites
Usually linear track of fibrosis with increased cellularity and hemosiderin-laden macrophages
If gelatin foam pledgets are present, they appear as acellular amphophilic material in center of biopsy site
There is chronic inflammatory response with giant cells around gelatin
Recent Excisional Sites
Usually easily identified due to fibrosis, hemorrhage, fat necrosis, and chronic inflammation
Cautery artifact is often present due to common use of electrocautery (e.g., BovieTM) to excise breast tissue
Electric field is generated in tissue
Cells and nuclei become elongated due to electrical potential across the cell membrane
Tissue with extensive cauterization loses recognizable histologic features and antigenicity
Other types of heat (e.g., ultrasonic coagulation or ablation) result in coagulative necrosis
Suture material is often present
Biodegradable suture (“catgut” suture) is monofilament made of strands of collagen
Usually ovoid in shape and brightly eosinophilic
Sutures are resorbed by exuberant chronic inflammatory infiltrate with foreign body giant cells
Collagen can have jagged edges, and elongated nuclei may be present
May be mistaken for heterotopic bone formation
Polyfilament sutures may also be present
Seromas and postoperative infections are possible complications
Remote Excisional Sites
Extent of healing varies greatly from patient to patient in terms of degree of response and time course
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree