9
Hypnotics, Sedatives, and Ethanol
Chapter 9 Hypnotics, Sedatives, and Ethanol is a combination of Chapter 17, Hypnotics and Sedatives and Chapter 23, Ethanol and Methanol from Goodman and Gilman’s The Pharmacological Basis of Therapeutics, 12th Edition. An understanding of the material in those chapters will be helpful in following the material presented in this chapter. In addition to the material presented here, the above chapters in the 12th Edition include:
• A detailed discussion of the pharmacological properties of benzodiazepines, including animal models of anxiety, the effects of benzodiazepines on the electroencephalogram (EEG) and sleep stages, the molecular targets of benzodiazepines, and GABAA receptor–mediated electrical events
• Table 17-1 Benzodiazepines: Names and Structures
• A discussion of miscellaneous sedative hypnotic drugs used less commonly today
• A detailed discussion of the management of insomnia
• The history of ethanol consumption details of the pharmacological effects of ethanol
In addition, the mechanisms of action of methanol and acute methanol poisoning, including treatment with ethanol and fomepizole are covered in this book Chapter 3 Clinical and Environmental Toxicity.
LEARNING OBJECTIVES
 Know the pharmacological effects, mechanisms of action, untoward effects, and therapeutic uses of benzodiazepines.
Know the pharmacological effects, mechanisms of action, untoward effects, and therapeutic uses of benzodiazepines.
 Know the pharmacological effects, mechanisms of action, untoward effects, and therapeutic uses of barbiturates.
Know the pharmacological effects, mechanisms of action, untoward effects, and therapeutic uses of barbiturates.
 Understand the management of insomnia.
Understand the management of insomnia.
 Know the effects of ethanol on physiological systems.
Know the effects of ethanol on physiological systems.
 Describe the issues of physical dependence and tolerance of chronic ethanol use.
Describe the issues of physical dependence and tolerance of chronic ethanol use.
 Understand the genetics of ethanol disposition.
Understand the genetics of ethanol disposition.
 Know the drugs used to treat alcoholism.
Know the drugs used to treat alcoholism.
DRUGS INCLUDED IN THIS CHAPTER
• Acamprosate (CAMPRAL)
• Alprazolam (XANAX)
• Amobarbital (AMYTAL)
• Butabarbital (BUTISOL, others)
• Carisoprodol (SOMA)
• Clomethiazole—not approved in the United States
• Chloral Hydrate (NOCTEC)
• Chlorazepate (TRANXENE, others)
• Chlordiazepoxide (LIBRIUM, others)
• Clonazepam (KLONIPIN)
• Diazepam (VALIUM, others)
• Disulfiram (ANTABUSE)
• Estazolam (PROSOM, others)
• Eszopiclone (LUNESTA)
• Etomidate (AMIDATE)
• Flumazenil (ROMAZICON)
• Flurazepam (DALMANE, others)
• Lorazepam (ATIVAN)
• Mephobarbital (MEBERAL)
• Meprobamate
• Methohexital (BREVITAL)
• Midazolam (VERSED)
• Nalmefene (REVEX)
• Naltrexone (REVIA, VIVITROL)
• Oxazepam (SERAX)
• Paraldehyde—no longer used in the United States
• Pentobarbital (NEMBUTAL)
• Phenobarbital (LUMINAL, others)
• Propofol (DIPRIVAN)
• Quazepam (DORAL)
• Ramelteon (ROZEREM)
• Secobarbital (SECONAL)
• Temazepam (RESTORIL)
• Thiopental (PENTOTHAL)
• Triazolam (HALCION)
• Zaleplon (SONATA)
• Zolpidem (AMBIEN)
MECHANISMS OF ACTION OF SEDATIVES, HYPNOTICS, AND DRUGS USED TO TREAT ALCOHOLISM
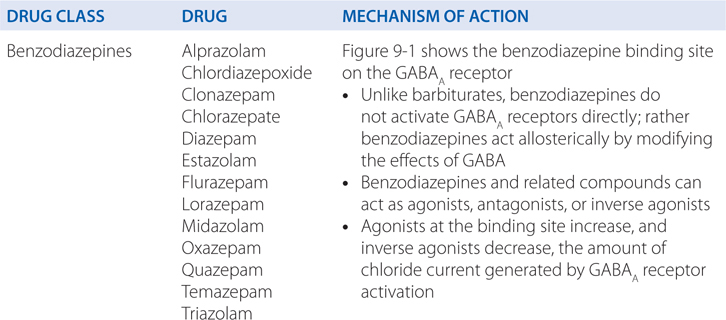
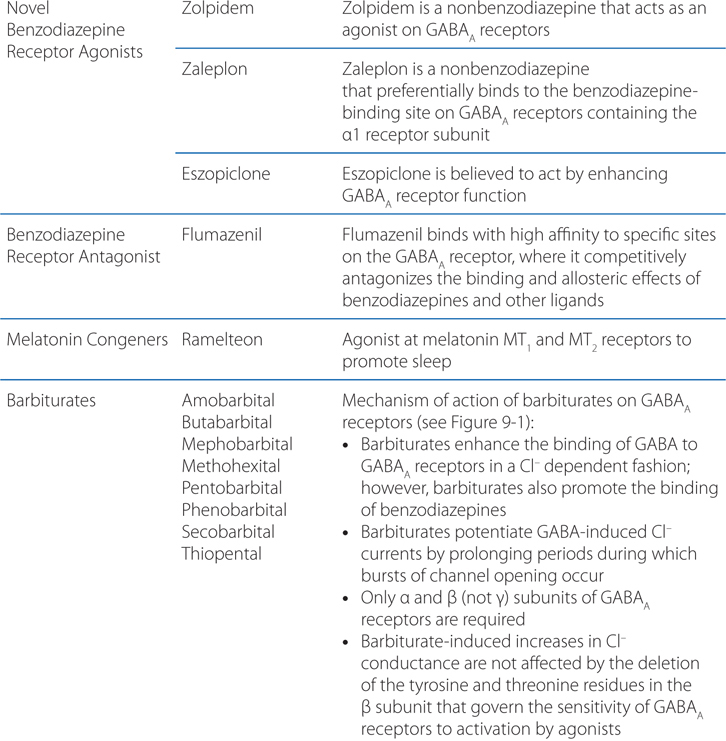
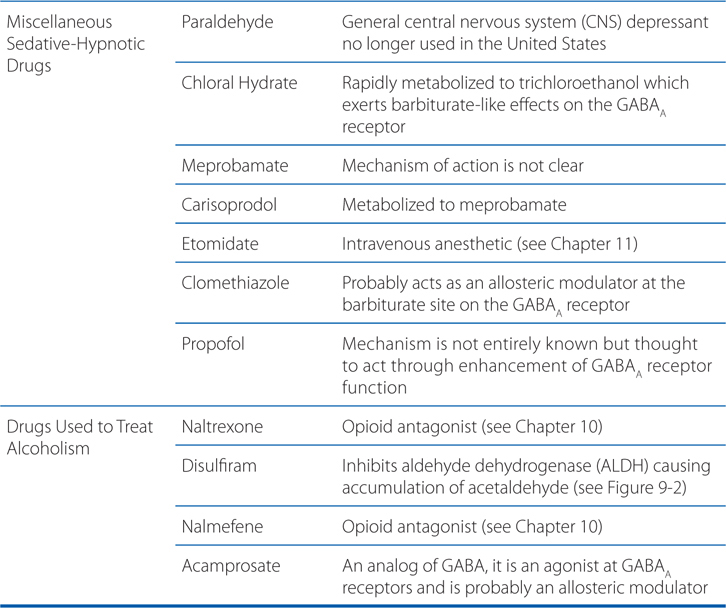
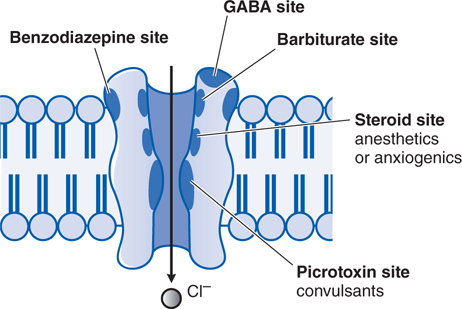
FIGURE 9-1 Pharmacologic binding sites on the GABAA receptor. (Reproduced with permission from Nestler EJ, Hyman SE, Malenka RC (eds). Molecular Neuropharmacology, 2nd ed. New York: McGraw-Hill, 2009, p 135. Copyright © 2009 by The McGraw-Hill Companies, Inc. All rights reserved.)
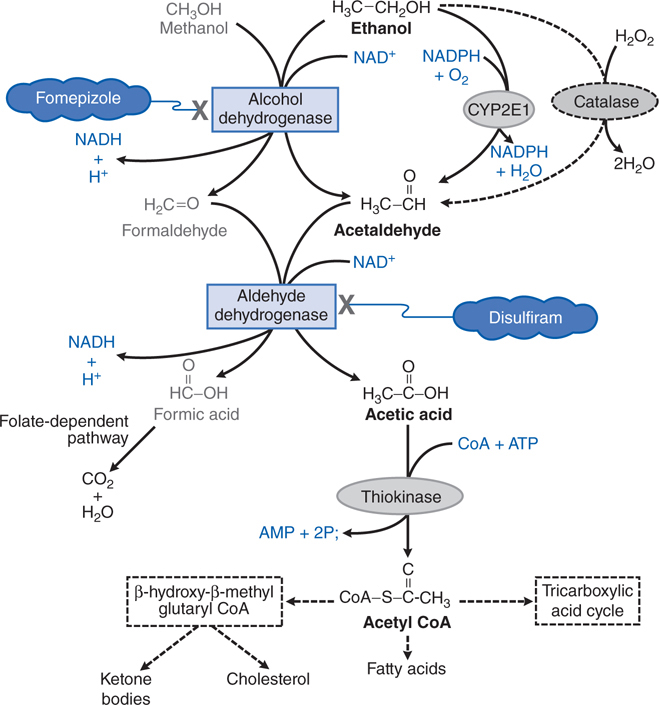
FIGURE 9-2 Metabolism of ethanol and methanol.
• Ultra-short acting—midazolam
• Short-acting agents (t1/2 <6 hours)—triazolam, the nonbenzodiazepine zolpidem (t1/2 ~2 hours), and eszopiclone (t1/2 5-6 hours)
• Intermediate-acting agents (t1/2 6-24 hours), including estazolam and temazepam
• Long-acting agents (t1/2 >24 hours), including flurazepam, diazepam, and quazepam
CATEGORIES OF INSOMNIA
• Transient insomnia lasts less than 3 days and usually is caused by a brief environmental or situational stressor
• Short-term insomnia lasts from 3 days to 3 weeks and is usually caused by a personal stressor such as illness, grief, or job problems
• Long-term insomnia is insomnia that has lasted for more than 3 weeks; no specific stressor may be identifiable
A 35-year-old woman comes to her physician complaining of not being able to sleep for the past week. She is prescribed zolpidem to be taken at bedtime.
a. What type of drug is zolpidem and what is its mechanism of action?
Zolpidem is a nonbenzodiazepine sedative-hypnotic drug approved for the short-term treatment of insomnia. Although the actions of zolpidem are due to agonist effects on GABAA receptors and generally resemble those of benzodiazepines, it produces only weak anticonvulsant effects in experimental animals, and its relatively strong sedative actions appear to mask anxiolytic effects in various animal models of anxiety.
b. What side effects should this woman be warned of?
After discontinuation of zolpidem, the beneficial effects on sleep reportedly persist for up to 1 week, but mild rebound insomnia on the first night also has occurred. Tolerance and physical dependence develop only rarely and under unusual circumstances. At therapeutic doses (5-10 mg), zolpidem infrequently produces residual daytime sedation or amnesia, and the incidence of other adverse effects (eg, GI complaints or dizziness) also is low. As with the benzodiazepines, large overdoses of zolpidem do not produce severe respiratory depression unless other agents (eg, ethanol) also are ingested. Hypnotic doses increase the hypoxia and hypercarbia of patients with obstructive sleep apnea.
c. What considerations should her physician be aware of when treating insomnia in this patient?
The categories of insomnia are shown in the Side Bar CATEGORIES OF INSOMNIA. This patient’s insomnia would be classified as short-term and hypnotics such as zolpidem should be used intermittently, perhaps even skipping a dose after 1 to 2 nights of good sleep. However, if her insomnia persists and becomes a long-term problem, it raises a new set of issues. Side effects of hypnotic agents may limit their usefulness for insomnia management (see Summary Table at the end of the chapter). The use of hypnotics for long-term insomnia is problematic for many reasons. Long-term hypnotic use leads to a decrease in effectiveness and may produce rebound insomnia on discontinuance. If a sedative-hypnotic has been used regularly for more than 2 weeks, it should be tapered rather than discontinued abruptly. In some patients on hypnotics with a short t1/2, it is easier to switch first to a hypnotic with a long t1/2 and then to taper. The onset of withdrawal symptoms from medications with a long t1/2 may be delayed. Consequently, the patient should be warned about the symptoms associated with withdrawal effects.
Hypnotics that act at GABAA receptors, including the benzodiazepine hypnotics and the newer agents zolpidem, zopiclone, and zaleplon, are preferred to barbiturates because they have a greater therapeutic index, are less toxic in overdose, have smaller effects on sleep architecture, and have less abuse potential. Compounds with a shorter t1/2 are favored in patients with sleep-onset insomnia but without significant daytime anxiety who need to function at full effectiveness during the day. These compounds also are appropriate for the elderly because of a decreased risk of falls and respiratory depression. However, the patient and physician should be aware that early-morning awakening, rebound daytime anxiety, and amnestic episodes could also occur. These undesirable side effects are more common at higher doses of the benzodiazepines.
A 23-year-old male college student is brought to the ER because he cannot be aroused. The patient has a history of depression and he has been acting depressed over his classes lately. The patient has a prescription for lorazepam for anxiety and insomnia. In the ER he is given flumazenil intravenously.
a. What type of drug is flumazenil and what is its role in treating a benzodiazepine overdose?
Flumazenil, the only member of this class, is an imidazobenzodiazepine that behaves as a specific benzodiazepine receptor antagonist. Flumazenil binds with high affinity to specific sites on the GABAA receptor, where it competitively antagonizes the binding and allosteric effects of benzodiazepines and other ligands. Flumazenil antagonizes both the electrophysiological and behavioral effects of agonist and inverse-agonist benzodiazepines. The drug is given intravenously.
The primary indications for the use of flumazenil are the management of suspected benzodiazepine overdose and the reversal of sedative effects produced by benzodiazepines administered during either general anesthesia or diagnostic and/or therapeutic procedures.
b. What cautions should be taken with this patient?
The administration of a series of small injections of flumazenil is preferred to a single bolus injection. A total of 1 mg flumazenil given over 1 to 3 minutes usually is sufficient to abolish the effects of therapeutic doses of benzodiazepines; patients with suspected benzodiazepine overdose should respond adequately to a cumulative dose of 1 to 5 mg given over 2 to 10 minutes; a lack of response to 5 mg flumazenil strongly suggests that a benzodiazepine is not the major cause of sedation. Additional courses of treatment with flumazenil may be needed within 20 to 30 minutes should sedation reappear. Flumazenil is not effective in single-drug overdoses with either barbiturates or tricyclic antidepressants. To the contrary, the administration of flumazenil in these settings may be associated with the onset of seizures, especially in patients poisoned with tricyclic antidepressants. Seizures or other withdrawal symptoms also may be precipitated in patients who had been taking benzodiazepines for protracted periods and in whom tolerance and/or dependence may have developed.
A 66-year-old man is brought to the ER with extreme anxiety, agitation, irritation, and confusion. It is learned that, because of early dementia, he recently did not renew his prescription for alprazolam, which he had been taking for the past 3 years for anxiety.
a. What is the likely cause of this patient’s change in mental status?
Chronic benzodiazepine use poses a risk for development of dependence and abuse. Mild dependence may develop in many patients who have taken therapeutic doses of benzodiazepines on a regular basis for prolonged periods. Withdrawal symptoms may include temporary intensification of the problems that originally prompted their use (eg, insomnia or anxiety). Dysphoria, irritability, sweating, unpleasant dreams, tremors, anorexia, and faintness or dizziness also may occur, especially when withdrawal of the benzodiazepine occurs abruptly. Hence, it is prudent to taper the dosage gradually when therapy is to be discontinued.
b. What are the options for treating this patient?
One option would be to reinstitute the alprazolam and once it has its calming effects, begin a slow tapering of the dose. Another option would be to begin a benzodiazepine with a longer t1/2 such as flurazepam and once it has its calming effects, discontinue its use and let the long half-life taper the effects and avoid withdrawal. Each of these options would depend on the ability of the patient or a caregiver to administer the drug.
A 43-year-old woman has been treated with secobarbital for insomnia for the past 10 years.
a. What distinguishes secobarbital from other barbiturates?
Table 9-1 shows the distinguishing features of selected barbiturates, including secobarbital. Secobarbital has a relatively short t1/2 compared to other barbiturates such as phenobarbital.
TABLE 9-1 Structures, Trade Names, and Major Pharmacological Properties of Selected Barbiturates
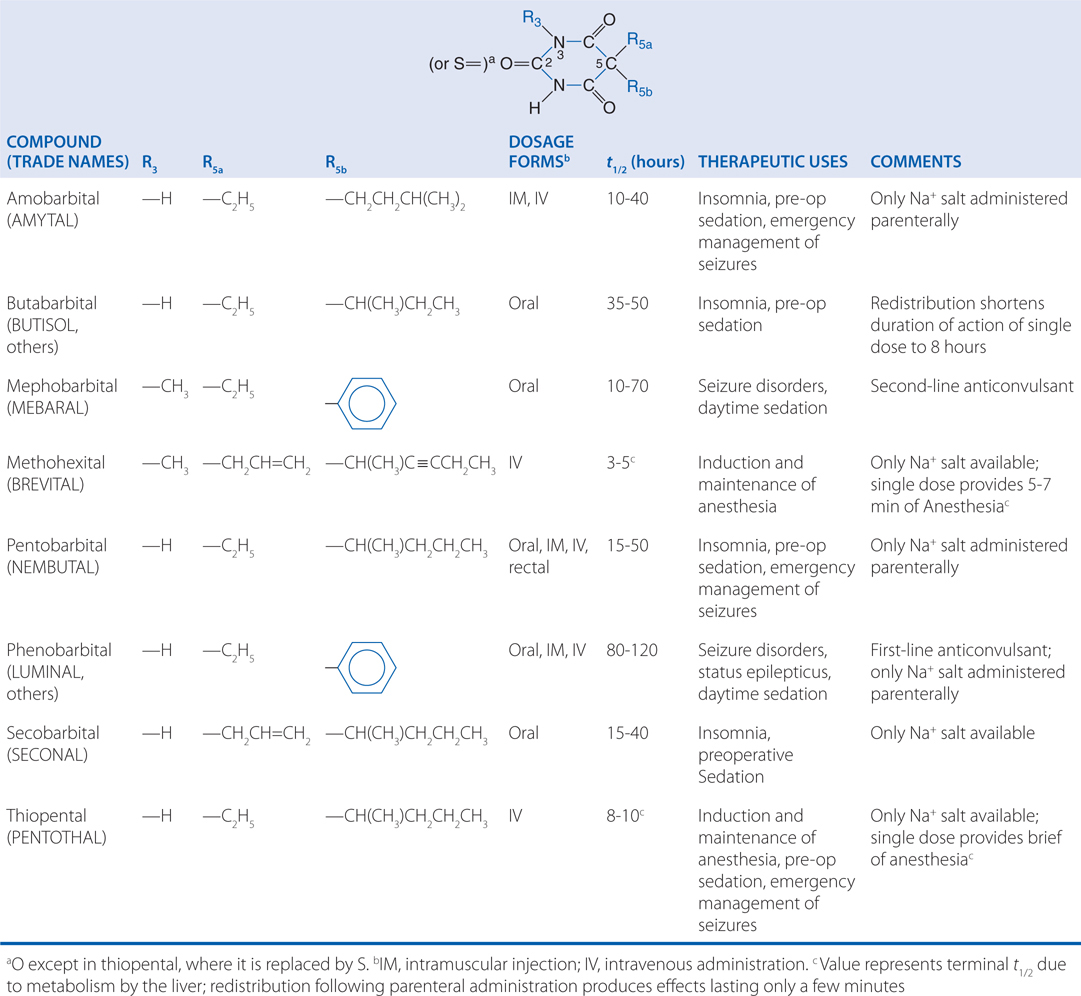
b. What is the mechanism of action of barbiturates?
See the Mechanisms of Action Table above. The barbiturates reversibly depress the activity of all excitable tissues. The barbiturates exert several distinct effects on excitatory and inhibitory synaptic transmission. For example, (–)-pentobarbital potentiates GABA-induced increases in chloride conductance and depresses voltage-activated Ca2+ currents at similar concentrations (<10 μM) in isolated hippocampal neurons. Barbiturates can produce all degrees of depression of the CNS, ranging from mild sedation to general anesthesia.
c. Why are barbiturates now not commonly used as sedatives?
The barbiturates were once used extensively as sedative-hypnotic drugs, but are associated with physical dependence. Except for a few specialized uses, they have been largely replaced by the much safer benzodiazepines.
d. Describe the tolerance and physical dependence that occurs with barbiturates.
Pharmacodynamic (functional) and pharmacokinetic tolerance to barbiturates can occur. The former contributes more to the decreased effect than does the latter. Tolerance to the effects on mood, sedation, and hypnosis occurs more readily and is greater than that to the anticonvulsant and lethal effects; thus, as tolerance increases, the therapeutic index decreases. Pharmacodynamic tolerance to barbiturates confers cross-tolerance to all general CNS-depressant drugs, including ethanol.
Chronic administration of barbiturates markedly increases the protein and lipid content of the hepatic smooth endoplasmic reticulum, as well as the activities of glucuronyl transferase and CYPs 1A2, 2C9, 2C19, and 3A4. The induction of these enzymes increases the metabolism of a number of drugs and endogenous substances, including steroid hormones, cholesterol, bile salts, and vitamins K and D. This also results in an increased rate of barbiturate metabolism, which partly accounts for the tolerance to barbiturates. Repeated administration, especially of phenobarbital, shortens the t1/2 of barbiturates that are metabolized as a result of the induction of microsomal enzymes.
Like other CNS depressant drugs, barbiturates are abused, and some individuals develop a dependence on them (see Chapter 14). Moreover, the barbiturates may have euphoriant effects.
Withdrawal from barbiturates can be serious, resulting in seizures and death.
e. What are the adverse effects that can be seen with the chronic use of barbiturates?
Drowsiness may last for only a few hours after a hypnotic dose of barbiturate, but residual CNS depression sometimes is evident the following day, and subtle distortions of mood and impairment of judgment and fine motor skills may be demonstrable. Residual effects also may take the form of vertigo, nausea, vomiting, or diarrhea, or sometimes may be manifested as overt excitement. The user may awaken slightly intoxicated and feel euphoric and energetic; later, as the demands of daytime activities challenge possibly impaired faculties, the user may display irritability and temper.
Rarely, exfoliative dermatitis may be caused by phenobarbital and can prove fatal; the skin eruption may be associated with fever, delirium, and marked degenerative changes in the liver and other parenchymatous organs.
Barbiturates combine with other CNS depressants to cause severe depression; ethanol is the most frequent offender, and interactions with first-generation antihistamines also are common.
Barbiturates competitively inhibit the metabolism of certain other drugs; however, the greatest number of drug interactions results from induction of hepatic CYPs and the accelerated disappearance of many drugs and endogenous substances (see answer to Case 9-4d above).
Because barbiturates enhance porphyrin synthesis, they are absolutely contraindicated in patients with acute intermittent porphyria or porphyria variegata.
DISTINGUISHING FEATURES OF FETAL ALCOHOL SYNDROME
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree