6 How essential oils enter the body
Introduction
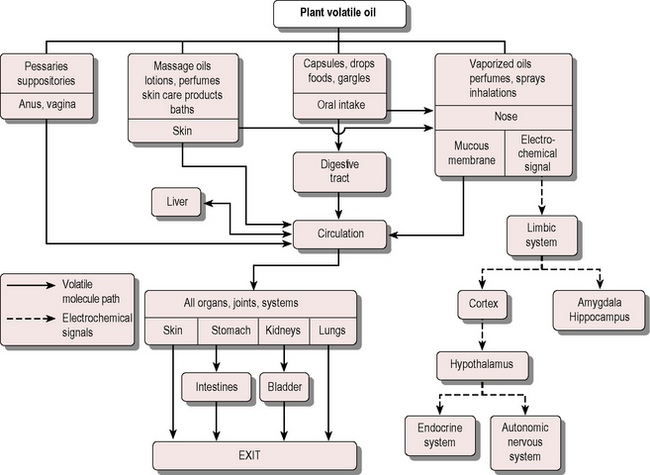
Essential oils follow three main pathways to gain entry to the body: ingestion, inhalation and absorption through the skin (Fig. 6.1). Ingestion is little used in the UK. Of the two remaining pathways, inhalation is a very effective method and indeed is regarded by some (e.g. Buchbauer 1988) as the only method truly deserving the name aromatherapy. However, topical application via the skin has also been found to be effective – the route selected depends on the problem being helped.
Inhalation
Access via the nasal passages is a speedy and effective route in the treatment of emotional problems such as stress and depression (and also some types of headache). This is because the nose has direct contact with the brain, which is responsible for triggering the effects of essential oils regardless of the route they use to gain access to it. The nose itself is not the organ of smell, but simply modifies the temperature and humidity of the inhaled air and collects any foreign matter that might be breathed in. The first cranial (olfactory) nerve is responsible for the sense of smell and serves the receptor cells, of which there are two groups of about 25 million, each occupying a small area (about 4 cm2) at the top of the nostrils (Van Toller 1993).
Methods of inhalation
Inhalation is an unobtrusive way of using essential oils in a healthcare setting. They may be given via a tissue, drops on the hands (in an emergency) a vaporizer etc., and all are effective in the appropriate situation. To select oils for particular conditions, see the tables in Ch. 4 and Appendix B.9 on the CD-ROM.
Steamers
• Ensure the patient’s eyes are kept closed and watch carefully for any adverse reaction, such as choking or coughing, which can happen if too many drops have been used or too deep a breath is taken.
• One drop only – with water of not too high a temperature – is adequate for asthmatics because the overpowering effect of the vapour (stronger because of the speedy evaporation referred to above) may have an adverse effect.
Baths
Treatment by putting oils into the bath is effective because not only do they come into gentle contact with the skin, they are also inhaled at the same time; thus a double benefit is derived. Note that undiluted essential oils can attack a plastic bath. For details, see Methods of percutaneous absorption, below.
Ethical considerations
When the effects required for a whole ward are the same for each occupant, e.g. keeping a ward free from infection or perhaps conducting a trial, the method is viable and effective; it can also be useful in the reduction of stress and insomnia, as well as in the destruction of germs. A few hospitals use vaporizers and diffusers in single-occupancy rooms only and not in general ward areas, as it is felt by some to be unethical to impose aromas (which may be disliked or unwanted by some) on other occupants. The same consideration should be given to the wearing of perfume and the use of scented cleaning materials, both of which can adversely affect the health of some people. Large vaporizer units used in hotels and offices are often run on commercial-grade essential oils and aromas to keep costs down, without taking into account the effect long-term exposure may have on people. It is already known that artificial perfumes and adulterated essential oils cause sensitivities in asthmatics and skin reactions in those susceptible to such effects (Box 6.1). ‘Environmental fragrancing’, as this practice is termed, is most advanced in the USA, where there is growing concern at the use of synthetic aromas. The liberty of the individual is an important consideration and, unlike shoppers irritated by ‘muzak’ or ‘fragrancing’ designed to alter their mood, hospital patients are not free to walk away from an unwanted environmental influence.
Absorption via the skin
Until the second half of the 20th century the skin was thought to be almost impermeable (Maibach & Marzulli 1977, Stoughton 1959). This idea still persists, even though the skin has been known for more than half a century to be a poor barrier to lipophilic substances (Brun 1952) and it has been shown that essential oils in a base oil applied to the skin are absorbed into the bloodstream (Jäger et al. 1992). Most chemicals are absorbed to some degree, and this is made use of in patch therapy, e.g. glyceryl trinitrate must penetrate the skin to reach the blood vessels and heart to treat angina, and many other substances – including oestradiol, scopolamine and nicotine – are administered in this way (Cleary 1993).
Transdermal delivery
Many drugs are unsuitable for use in therapeutic transdermal delivery systems owing to their low ability to permeate the skin, so the use of penetration-enhancing agents is advantageous; various studies suggest that essential oils offer a useful selection of safe penetration enhancers to aid topical drug delivery. Eucalyptus and chenopodium essential oils caused a 30-fold increase in the drug 5-fluorouracil (5-FU) permeability coefficient using excised human skin; animal studies showed enhanced skin penetration for some drugs with eucalyptus oil, camphor and limonene; and in laboratory tests on excised human skin the penetration of 5-FU was increased with aniseed oil (2.8 times), ylang oil (7.8 times) and eucalyptus oil (34 times) (Williams & Barry 1989).The skin permeation of the neuroleptic drug haloperidol was increased in the presence of cineole and (+)-limonene, but that of chlorpromazine was not; in fact (+)-limonene reduced it (Almiral et al. 1996); terpenes have been shown to have an enhancing effect on the transdermal permeation of hydrophilic drugs, and chlorpromazine is more lipophilic than haloperidol. The principal component of eucalyptus oil was investigated to determine whether 1,8-cineole could be detected in effective amounts in skeletal muscles after dermal application; the bioavailability of 1,8-cineole was 320% greater when using an applicator than with an occlusive dressing (Weyers & Brodbeck 1989).
Takayama and Nagai (1994) studied the promoting effects of terpenes present in essential oils on the percutaneous absorption of indomethacin from hydrogels in rats in vivo and found that absorption was remarkably enhanced by cyclic monoterpenes such as limonene, terpinene and terpinolene. It was noted that the terpenes had a strong fluidizing effect on the lipid bilayer structure, and (+)-limonene in the presence of ethanol changed the barrier structure of the skin, accelerating the transfer of ethanol, and thus the permeation of indomethacin was promoted because of its affinity with alcohol.
Sesquiterpenes also have been shown to increase 5-FU absorption across human (cadaver) skin; the increase was thought to be brought about by disrupting intercellular lipid bilayers and by forming complexes with 5-FU: sesquiterpenes with polar functional groups produced the greatest improvements in absorption (Cornwall & Barry 1994). The mechanisms by which penetration enhancers increase the permeability of the stratum corneum are discussed by Cornwall et al. (1996).
Cinnamon oil, clove oil and galangal were studied as percutaneous enhancers for benzoic acid and it was found that skin penetration was significantly enhanced by all three volatile oils (Shen et al. 2001). in vitro tests with cajuput, cardamom, melissa, myrtle, niaouli and orange oils on the permeation of estradiol through hairless mouse skin showed that niaouli was the best permeation enhancer. The whole oil of niaouli was a better activity promoter than its single isolated compounds, and the data demonstrated complex terpene mixtures to be potent enhancers of transdermal penetration for moderately lipophilic drugs such as estradiol (Monti et al. 2002). Clove oil tested on the transdermal delivery of ibuprofen in rabbits showed significant enhancement in vitro and a lesser effect in vivo; the enhanced delivery was attributed to the principal components eugenol and acetyl eugenol (Shen et al. 2007). Basil oil was found to be a promising penetration enhancer for the drug labetolol (Jain et al. 2008).
The skin as a water barrier
Water comprises 90% of any cell, and therefore the skin has developed as a barrier specifically to resist water; nevertheless, it is slightly permeable to water-soluble substances, to water itself and to lipids (Riviere 1993). The absorption of drugs and poisons through the skin was studied by Macht (1938) and there has been a considerable amount of research on pesticides and the skin. Pesticides, which dissolve in essential oils, are lipid-like and can therefore penetrate the skin – every farmer is aware of this health hazard and many people are killed each year by pesticides, mostly in developing countries. The amount absorbed through human skin varies enormously: for example, less than 1% of cypermethrin pesticide is absorbed, whereas up to 65% of the antifungal agent benzoic acid may penetrate the skin (Hotchkiss 1994).
The skin’s success as a barrier is due in the main to the stratum corneum, the tough and durable, self-repairing keratinized layer, which is 20 layers of dead cells thick. Once a chemical gets past the epidermis – the only great obstacle – the rest of the journey into the body is easy, because of the presence of lipids in all cell membranes. For example, the antibacterial substance hexachlorophene is absorbed through the skin and was shown in 1969 to cause microscopically visible brain damage in rats (Winter 1984 p. 138) and chloasma in humans; in the 1970s hexachlorophene was used as an antiseptic in baby soaps and talcum powders, causing brain damage and even death in some babies after it had penetrated the skin (Jackson 1993). The lipid solubility of essential oil components allows these compounds to cross the blood–brain barrier (where certain substances are held back by the endothelium of cerebral capillaries) and make contact with the fluids around the brain (Anthony & Thibodeau 1983).
Many factors dictate the rate and quantity at which any given substance penetrates the skin, but it is now generally recognized that the skin is a semi-permeable membrane susceptible of penetration by substances to a greater or lesser degree (Lexicon Vevy 1993a). The physicochemical properties of the molecules, such as the molecular weight, spatial arrangement, polarity, optical activity, liposolubility, coefficients of diffusion and dissociation, are fundamental to skin penetration. Mills (1993) states that an advantage of the percutaneous route for remedies is the avoidance of the ‘first-pass liver’ effect, i.e. they are not subject to immediate metabolization by the liver as they are with oral administration.
The skin as a gateway
Because of their solubility in the lipids found in the stratum corneum, lipophilic substances (such as essential oils) are considered to be easily absorbed. The absorption of organic compounds with anionic or cationic groups (weak acids and alkalis) takes place when they are found in undissociated form – then they are more lipophilic than when dissociated; it also depends on their dissociation constant and on the pH of the substance and of the skin. The majority of essential oils and their components pass through the skin and the organism (Valette 1945) and can be detected in exhaled air within 20–60 minutes (Katz 1947). Some examples of the times recorded are: 1,8-cineole and α-pinene take 20 minutes; eucalyptus, eugenol, linalyl acetate, geranyl acetate, anethole and thyme oil take between 20 and 40 minutes; bergamot, aniseed and lemon oils take between 40 and 60 minutes; true lavender, pine, geranium and citronella oils and cinnamaldehyde take between 60 and 80 minutes; coriander, rue and peppermint oils, geraniol and citrals take up to 2 hours.
The main factors affecting the penetration of the skin by essential oils are detailed below.
Intrinsic factors
• Area of skin. The very large area of the skin – in the region of 2 m2 – makes it possible for a significant quantity of essential oils to be applied and so taken into the body. If a set quantity of essential oil in a carrier is applied to a small area of skin, then less will enter than if the same quantity were to be applied to a greater area.
• Thickness and permeability of the epidermis. On palmar and plantar skin sites where the epidermis is quite thick and there are no oil glands, the time taken to cross the skin is longer, especially for any lipid-soluble components. There is less resistance to water-soluble components, however, e.g. garlic placed on the feet is soon detected on the exhaled breath. Easy penetration may occur on parts of the body where the skin is thinner, e.g. behind the ears, on the eyelids and inside the wrist. The skin regions of the legs, buttocks, trunk and abdomen are less permeable than are those of the soles, palms, forehead, scalp and armpits (Balacs 1993).
• Gland openings and follicles. Hydrophilic molecules can find a path through the skin using the sweat glands; lipophilic molecules may use the sebaceous glands as a pathway, also travelling between the cells through the fatty cement and through the cells themselves, all of which contain lipids (Lexicon Vevy 1993b). The skin of the forehead and scalp contains numerous oil glands, and here the epidermis is thinner. This again makes for easy penetration of lipophilic substances, although the water layer on the skin must present a partial barrier for the lipophilic molecules. The number of follicles and sweat glands is another factor: generally speaking, the more openings the speedier the access. When sweating, because of a fever or after a sauna, for example, the body is exuding and ingress of essential oils is hindered.
• Reservoirs. Essential oils, being lipid soluble, gain access to lipid-rich areas of the body (Buchbauer 1993), therefore it is possible that they may be sequestered (stored apart) in the body, as happens in the plants that produce them. If so, there may be reservoirs of essential oils (or at least of some of their constituent molecules) in the outer layers of the epidermis and subcutaneous fat, and these may persist for some time. It is considered that lipophilic components can, at least temporarily, be retained in this layer and consequently will not be available for rapid diffusion to other adjacent levels (Lexicon Vevy 1993b). Subcutaneous fat has a poor blood supply, and although essential oils are slow to enter they probably tend to stay there for a long time. A Dutch Government Commission report in 1983 showed that many MAC (maximum acceptable concentrations) for toxic chemicals failed to take into account the significant physiological differences between the sexes. Women’s skin is more permeable to toxic chemicals than that of men, and because they carry more fat, their body levels of fat-soluble chemicals are generally higher and take longer to disperse (Eisberg 1983).
• Enzymes. Enzymes in the skin can activate and inactivate many drugs and foreign compounds. They can also activate and inactivate the body’s own natural chemicals, such as hormones, steroids and inflammatory mediators. The activities of these skin enzymes may vary greatly between individuals and with age (Hotchkiss 1994). The skin contains many enzymes and therefore provides a ‘laboratory’ where metabolism can take place. Certainly some enzymes will effect a change in some essential oil molecules, and even a slight change in molecular shape will mean a change in the effect on the body. In the case of some phthalic esters, enzymatic action effects complete metabolization during skin absorption; enzymes in the skin can either activate or inactivate drugs and other alien compounds, and there is great variation between individuals and with age. Bacterial action breaks down the triacylglycerides in sebum to organic free fatty acids and incompletely esterified glycerol derivatives, and it is reasonable to suppose that similar sorts of processes may happen with the essential oils.
• Damaged skin. Broken, inflamed and diseased skin is a poor barrier and ingress is rapid through cuts, abrasions, ulcers, psoriasis, burns etc. Aged skin and skin dehydrated through exposure to sunlight does not accept substances easily: some dermatological problems (e.g. ichthyosis) may also have this same effect.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree