Homeostasis and the Stress Response
Stress is one of the most cited concepts in biomedical literature. Whether physical, mental, or emotional, stress has the potential to be positive or negative depending on the individual and the situation. From a positive aspect, stress can preserve life, but if left unresolved, maladaption, and even death can occur. The result of stress is dependent on many factors such as type, duration, adaptation, intensity, and coping abilities. The physiologic pathways and pathophysiologic effects of stress can be evaluated objectively and are described in this chapter.
● Physiologic Concepts
DEFINITION OF STRESS
Stress has been defined in many different ways for over 100 years. The modern concept of stress assumes that humans live in a world that has multiple threats (e.g., terrorism) and challenges (e.g., living in a 24-7 world) and that the everchanging demands of daily life require constant psychological, behavioral, and physiologic adjustment. Thus, stress can be defined as anything that disrupts equilibrium, or any demand that exceeds the body’s ability to cope. Stress is a subjective experience that can have negative health consequences.
TYPES OF STRESSORS
Stressors include a wide variety of factors ranging from psychological (e.g., speech anxiety, worry, and mental anguish) and environmental (e.g., natural disasters, socioeconomic status) to physical (e.g., exercise, trauma, and illness) and
immunologic (e.g., infection, physical disease). Stressors can be pleasant (“eustress”), as in the case of a wedding or graduation, or unpleasant (“distress”), such as losing a job. They also vary in duration (i.e., acute vs. chronic) and frequency (e.g., daily vs. monthly). Acute stressors are temporary and identifiable. Chronic stressors are long term and may not be as easily identified. Constant exposure to a stressor tends to synthesize the individual to the situation so that the source of the stress may not be as obvious. The low level of stress may become a way of life and negatively impact the health of the individual.
immunologic (e.g., infection, physical disease). Stressors can be pleasant (“eustress”), as in the case of a wedding or graduation, or unpleasant (“distress”), such as losing a job. They also vary in duration (i.e., acute vs. chronic) and frequency (e.g., daily vs. monthly). Acute stressors are temporary and identifiable. Chronic stressors are long term and may not be as easily identified. Constant exposure to a stressor tends to synthesize the individual to the situation so that the source of the stress may not be as obvious. The low level of stress may become a way of life and negatively impact the health of the individual.
A stressor does not always need to be physically present for a person to experience its negative consequences, as in the case of posttraumatic stress disorder (PTSD). Although they occurred in the past, remembered stressors, such as the events of September 11, 2001 or the death of a spouse, can be traumatic enough to provoke a stress response just from being recalled. While occasional stress exposure can provide stimulation and intellectual challenge, prolonged stress challenges the body’s ability to maintain physical and emotional homeostasis and is associated with negative bodily responses.
HOMEOSTASIS
Homeostasis was defined by Walter B. Cannon, a noted American physiologist of the early 20th century, as the maintenance of the physiologic internal environment. Stressors threaten the body’s ability to maintain physiologic homeostasis. The body responds to any change in internal conditions with reflexes designed to return itself to the previous state. Homeostasis is usually accomplished by activation of a negative feedback cycle. An initiating stimulus (i.e., the stressor) causes activation of a response, which then directly or indirectly leads to a lessening of the initiating stimulus. This feedback loop allows the body to remain in a dynamic steady state, whereby it continually adjusts to maintain its internal composition and function. Figure 6-1 shows a negative feedback cycle for a physical or mental stressor.
Cannon also noted the role that homeostasis plays in species survival. The fight-or-flight response, proposed in the early 1900s, is a prototypical mammalian stress response in which an organism (such as a human) either fights or flees when faced with a threat (such as a tiger) in order to survive. Thus, stressors trigger a coordinated cascade of biological and behavioral responses that are designed to ensure the safety and well-being of the organism. Under acute conditions, this biobehavioral cascade can be incredibly adaptive in preventing harm. In contrast, continued exposure to stressors and their consequent physiologic end products can result in damage to the body. These biobehavioral cascades are discussed in the following section.
NERVOUS SYSTEM AND HORMONAL RESPONSES TO STRESS
The response to stress involves activation of the sympathetic nervous system (SNS) and the release of various hormones and peptides, including those of
the hypothalamic-pituitary-adrenal (HPA) axis, the endogenous opioid system, arginine vasopressin (AVP), and oxytocin. The stress response also affects the release of growth and reproductive hormones. These responses prepare the body to cope with or overcome the stressor and are important for the survival and well-being of the organism.
the hypothalamic-pituitary-adrenal (HPA) axis, the endogenous opioid system, arginine vasopressin (AVP), and oxytocin. The stress response also affects the release of growth and reproductive hormones. These responses prepare the body to cope with or overcome the stressor and are important for the survival and well-being of the organism.
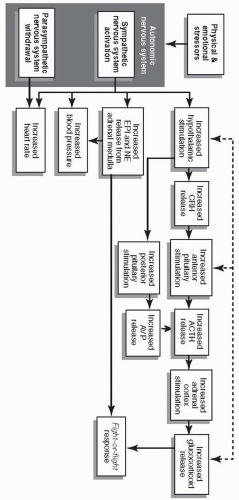
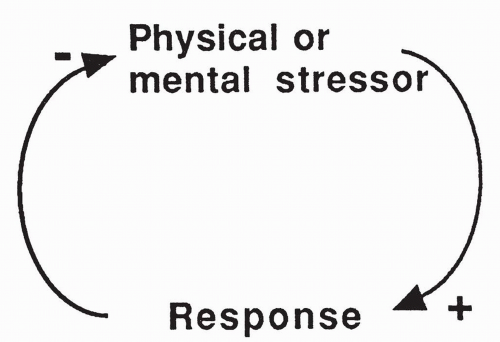 FIGURE 6-1 A stressor causes a response that acts in a negative feedback manner to reduce the impact of the original stressor. |
The Sympathetic Nervous System
The fight-or-flight response begins with the activation of the SNS, a branch of the autonomic nervous system (ANS) (Fig. 6-2). Immediately following stressor exposure, the SNS responds with the release of the catecholamines epinephrine and norepinephrine from sympathetic neurons and the adrenal medulla, located in the center of the adrenal glands.
The responses to catecholamines are similar whether they are released from nerves or from the adrenal medulla. However, catecholamines released from the adrenal gland are rapidly metabolized and thus show more limited effects. Effects of the catecholamines include the following:
Circulating and neurally released norepinephrine binds to receptors identified as alpha1 and alpha2. Binding to alpha1 receptors present on most vascular smooth muscle cells causes the muscle to contract resulting in decreased blood flow to organs supplied by those vascular beds. As a result, sympathetic activation causes a decrease in blood flow to the organs of the gastrointestinal (GI) tract, the skin, and the kidneys. This ensures maximum blood flow to the brain, heart, and skeletal muscles in times of stress. Norepinephrine also binds to receptors on the smooth muscle of the GI tract causing relaxation of the muscle and thereby slowing digestion and GI motility.
Norepinephrine release causes an increase in plasma glucose levels by increasing the breakdown and release of glucose storage forms in the liver and skeletal muscles, thereby providing the body with a ready supply of energy.
Norepinephrine released by sympathetic nerves innervating the eye causes dilation of the pupil, preparing the body for any type of attack or surprise.
Circulating and neurally released epinephrine acts by binding to alphareceptors and beta-receptors, identified as β1 and β2. By binding to β1 receptors on the heart, epinephrine causes an increase in the heart rate and an increase in cardiac contractility, both of which serve to increase the cardiac output during stress.
Epinephrine binding to β2 receptors in the liver and skeletal muscle causes an increase in glucose release, resulting in increased glucose available for all cells to use if fight or flight is necessary.
Epinephrine binding to β2 receptors present on bronchiolar smooth muscle increases airflow to the lungs by relaxing the muscle, thereby opening up the air passages and facilitating oxygenation of blood for tissues that may be called on during a stressful situation.
The Hypothalamic-Pituitary Hormones
The hypothalamus is the primary structure in the brain responsible for maintaining physiologic homeostasis. It is affected by both physical and psychological stressors. Considered the master endocrine (hormonal) gland of the body, the hypothalamus controls the secretion of several important hormones. The hypothalamus is also connected through a wide neural network to other structures throughout the cerebral cortex and the limbic system. The hypothalamus is the part of the brain that is important in controlling water balance, body temperature, body growth, and hunger (Chapter 9). It is involved in monitoring and responding to feelings of rage, passion, and fear. The hypothalamus also integrates the responses of the sympathetic and parasympathetic systems. Stress affects the hypothalamus and therefore the release of several important hormones and neurotransmitters.
Overview of HPA Axis Activation
SNS activation by stress stimulates the HPA axis (see Fig. 6-2). HPA axis activation begins with the secretion of corticotropin-releasing hormone (CRH) from the paraventricular nucleus of the hypothalamus into the hypothalamic-pituitary portal blood flow system, which in turn stimulates the secretion of adrenocorticotropic hormone (ACTH) from the anterior pituitary, as well as AVP from the posterior pituitary gland. While AVP acts centrally to support the fight-or-flight response, ACTH circulates to the cortex of the adrenal glands to stimulate glucocorticoid release, including release of the corticosteroids (e.g., cortisol, corticosterone). Corticosteroids themselves regulate continued HPA axis function through a negative feedback loop by dampening further CRH release from the hypothalamus and ACTH release from the anterior pituitary gland. Ultimately, these stress hormones mobilize energy stores so that an organism can adapt to the stressor.
Cortisol
Cortisol is the primary corticosteroid associated with stress. It can be measured in blood, urine, feces, and saliva, and has multiple effects on the body, many
of which allow an individual to cope with and survive a stressor. The effects of cortisol include the following:
of which allow an individual to cope with and survive a stressor. The effects of cortisol include the following:
Stimulates new formation of glucose (gluconeogenesis), which increases the availability of glucose as an energy source in times of immediate need.
Stimulates the breakdown of stored energy molecules such as fat, protein, and carbohydrate to allow mobilization of energy if immediate fight or flight is required.
Primes the body to respond to all stressors by promoting sympathetic responses, including those geared toward enhancing cardiac output and maintaining blood pressure.
Appears to affect the central nervous system. When confronted by a stressor, arousal is initiated and maintained, and the individual becomes cognitively and emotionally equipped to respond.
Regulates further HPA axis activation through a negative feedback loop by returning CRH release from the hypothalamus and ACTH release from the anterior pituitary gland toward baseline levels (see Fig. 6-2).
Stimulates gastric acid secretion, which may lead to a breakdown of the gastric mucosa.
Affects the release of other hypothalamic-releasing factors and hormones. It inhibits the gonadotropin-releasing factors that control ovulation in women and sperm production and testosterone synthesis in men.
Appears to also stimulate the release of the hypothalamic hormone somatostatin, an inhibitor of growth hormone (GH) release. It is possible that these effects of cortisol contribute to the reproductive dysfunction and growth deficiencies seen in some individuals with long-term stress.
A high level of cortisol has many effects on the immune and inflammatory reactions, all of which are geared toward reducing inflammation and immune function. For instance, cortisol inhibits the production and release of all white blood cells, blocks B-cell and T-cell functions, and blocks the production of interleukins, which allow for communication among white blood cells. Cortisol reduces white blood cell accumulation at sites of injury or infection, causing a reduction in the usual inflammatory reactions. As a result of its effects on the immune system, elevated levels of cortisol can cause an increased susceptibility to infection and may delay or block healing. Because of these negative effects, it is often wondered why cortisol release is stimulated during states of infection or tissue injury. It may be that a short-term release of cortisol helps to limit damage to tissues caused by inflammation, and it is only with chronic stress that harmful effects of prolonged immunosuppression become obvious.
The Endogenous Opioid Peptides
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree