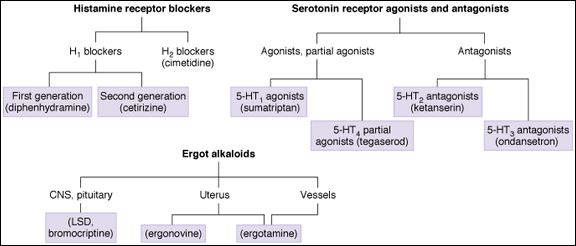
receptors. They are included in this chapter because of their effects on serotonin receptors and on smooth muscle. Peptide and eicosanoid autacoids are discussed in Chapters 17 and 18. Nitric oxide is discussed in Chapter 19.
High-Yield Terms to Learn
Acid-peptic disease Disease of the upper digestive tract caused by acid and pepsin; includes gastroesophageal reflux, erosions, and ulcers Autacoids Endogenous substances with complex physiologic and pathophysiologic functions that have potent nonautonomic pharmacologic effects when administered as drugs; commonly understood to include histamine, serotonin, prostaglandins, and vasoactive peptides Carcinoid A neoplasm of the gastrointestinal tract or bronchi that may secrete serotonin and a variety of peptides Ergotism (“St. Anthony’s fire”) Disease caused by excess ingestion of ergot alkaloids; classically an epidemic caused by consumption of grain (eg, in bread) that is contaminated by the ergot fungus Gastrinoma A tumor that produces large amounts of gastrin; associated with hypersecretion of gastric acid and pepsin leading to ulceration IgE-mediated immediate reaction An allergic response, for example, hay fever, angioedema, caused by interaction of an antigen with IgE antibodies on mast cells; results in the release of histamine and other mediators of allergy Oxytocic A drug that causes contraction of the uterus Zollinger-Ellison syndrome Syndrome of hypersecretion of gastric acid and pepsin, often caused by gastrinoma; it is associated with severe acid-peptic ulceration and diarrhea
Histamine
Histamine is formed from the amino acid histidine and is stored in high concentrations in vesicles in mast cells, enterochromaffin cells in the gut, some neurons, and a few other cell types. Histamine is metabolized by the enzymes monoamine oxidase and diamine oxidase. Excess production of histamine in the body (eg, in systemic mastocytosis) can be detected by measurement of imidazole acetic acid (its major metabolite) in the urine. Because it is released from mast cells in response to IgE-mediated (immediate) allergic reactions, this autacoid plays an important pathophysiologic role in seasonal rhinitis (hay fever), urticaria, and angioneurotic edema. Histamine also plays an important physiologic role in the control of acid secretion in the stomach and as a neurotransmitter.
Receptors and Effects
Two receptors for histamine, H1 and H2, mediate most of the peripheral actions; 2 others (H3, H4) have also been identified (Table 16-1). The triple response, a classic demonstration of histamine effect, is mediated mainly by H1 and H2 receptors. This response involves a small red spot at the center of an intradermal injection of histamine surrounded by a red edematous wheal.
TABLE 16-1 Some histamine and serotonin receptor subtypes.a
Receptor Subtype Distribution Postreceptor Mechanisms Prototypic Antagonist H1
Smooth muscle Gq;  IP 3, DAG
IP 3, DAG
Diphenhydramine H2
Stomach, heart, mast cells Gs;  cAMP
cAMP
Cimetidine H3
Nerve endings, CNS Gi;  cAMP
cAMP
Clobenpropitb
H4
Leukocytes Gi;  cAMP
cAMP
— 5-HT 1D
Brain Gi;  cAMP
cAMP
— 5-HT2
Smooth muscle, platelets Gq;  IP3, DAG
IP3, DAG
Ketanserin 5-HT3
Area postrema (CNS), sensory and enteric nerves Ligand-gated cation channel Ondansetron 5-HT4
Presynaptic nerve terminals in the enteric nervous system Gs;  cAMP
cAMP
Tegaserod (partial agonist)
aMany other serotonin receptor subtypes are recognized in the CNS. They are discussed in Chapter 21.
bClobenpropit is investigational.
cAMP, cyclic adenosine phosphate; CNS, central nervous system; DAG, diacylglycerol; IP3, inositol trisphosphate.
H1 Receptor
This Gq-coupled receptor is important in smooth muscle effects, especially those caused by IgE-mediated responses. Inositol trisphosphate (IP 3) and diacylglycerol (DAG) are the second messengers. Typical responses include pain and itching in the skin, bronchoconstriction, and vasodilation, the latter caused by release of nitric oxide. Capillary endothelial cells, in addition to releasing nitric oxide (NO) and other vasodilating substances, also contract, opening gaps in the permeability barrier and leading to the formation of local edema. These effects occur in allergic reactions and in mastocytosis.
H2 Receptor
This Gs-coupled receptor mediates gastric acid secretion by parietal cells in the stomach. It also has a cardiac stimulant effect. A third action is to reduce histamine release from mast cells—a negative feedback effect. These actions are mediated by activation of adenylyl cyclase, which increases intracellular cyclic adenosine monophosphate (cAMP).
H3 Receptor
This Gi-coupled receptor appears to be involved mainly in presynaptic modulation of histaminergic neurotransmission in the central nervous system (CNS). Food intake and body weight increase in H3-receptor knockout animals. In the periphery, it appears to be a presynaptic heteroreceptor with modulatory effects on the release of other transmitters (see Chapter 6).
H4 Receptor
The H4 receptor is located on leukocytes (especially eosinophils) and mast cells and is involved in chemotactic responses by these cells. Like H3, it is Gi coupled.
Clinical Use
Histamine has no therapeutic applications, but drugs that block its effects at H1 and at H2 receptors are very important in clinical medicine. No antagonists of H3 or H4 receptors are currently available for clinical use.
Histamine H1 Antagonists
Classification and Prototypes
A wide variety of antihistaminic H1 blockers are available from several different chemical families. Two major subgroups or “generations” have been developed (see the drug classification at the beginning of the chapter). The older members of the first-generation agents, typified by diphenhydramine, are highly sedating agents with significant autonomic receptor-blocking effects. A newer subgroup of first-generation agents are less sedating and have much less autonomic effect. Chlorpheniramine and cyclizine may be considered prototypes. The second-generation H1 blockers, typified by cetirizine, fexofenadine, and loratadine, are far less lipid soluble than the first-generation agents and have further reduced sedating and autonomic effects. Because they have been developed for use in chronic conditions, all H1 blockers are active by the oral route. Several are promoted for topical use in the eye or nose. Most are metabolized extensively in the liver. Half-lives of the older H1 blockers vary from 4-12 h. Most second-generation agents (eg, fexofenadine, cetirizine, loratadine) have half-lives of 12-24 h.
Mechanism and Effects
H1 blockers are competitive pharmacologic antagonists at the H1 receptor; these drugs have no effect on histamine release from storage sites. They are more effective if given before histamine release occurs.
Because their structure closely resembles that of muscarinic blockers and  -adrenoceptor blockers, many of the first-generation agents are potent pharmacologic antagonists at these autonomic receptors. A few also block serotonin receptors. As noted, most older first-generation agents are sedating, and some—not all—first-generation agents have anti-motion sickness effects. Many H1 blockers are potent local anesthetics.
-adrenoceptor blockers, many of the first-generation agents are potent pharmacologic antagonists at these autonomic receptors. A few also block serotonin receptors. As noted, most older first-generation agents are sedating, and some—not all—first-generation agents have anti-motion sickness effects. Many H1 blockers are potent local anesthetics.
H1-blocking drugs have negligible effects at H2 receptors.
Clinical Use
H1 blockers have major applications in allergies of the immediate type (ie, those caused by antigens acting on IgE antibody-sensitized mast cells). These conditions include hay fever and urticaria.
Diphenhydramine, dimenhydrinate, cyclizine, meclizine, and promethazine are used as anti-motion sickness drugs. Diphenhydramine is also used for management of chemotherapy-induced vomiting.
Adverse effects of the first-generation H1 blockers are sometimes exploited therapeutically (eg, in their use as hypnotics in over-the-counter sleep aids).
Toxicity and Interactions
Sedation is common, especially with diphenhydramine and promethazine. It is much less common with second-generation agents, which do not enter the CNS readily. Antimuscarinic effects such as dry mouth and blurred vision occur with some first-generation drugs in some patients. Alpha-adrenoceptor blockade, which is significant with phenothiazine derivatives such as promethazine, may cause orthostatic hypotension.
Interactions occur between older antihistamines and other drugs with sedative effects (eg, benzodiazepines and alcohol). Drugs that inhibit hepatic metabolism may result in dangerously high levels of certain antihistaminic drugs that are taken concurrently. For example, azole antifungal drugs and certain other CYP3A4 inhibitors interfere with the metabolism of astemizole and terfenadine, 2 second-generation agents that have been withdrawn from the US market because high plasma concentrations of either antihistamine can precipitate lethal arrhythmias.
Histamine H2 Antagonists
Classification and Prototypes
Four H2 blockers are available; cimetidine is the prototype. Ranitidine, famotidine, and nizatidine differ only in having fewer adverse effects than cimetidine. These drugs do not resemble H1 blockers structurally. They are orally active, with half-lives of 1-3 h. Because they are all relatively nontoxic, they can be given in large doses, so that the duration of action of a single dose may be 12-24 h. All four agents are available in oral over-the-counter formulations.
Mechanism and Effects
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


