High-Grade Serous Adenocarcinoma
Martin Köbel, MD
Blake C. Gilks, MD, FRCPC
Key Facts
Clinical Issues
Bilateral (60%)
Mean: 6th to 7th decade
Stage dependent; 30-40% overall 5-year survival
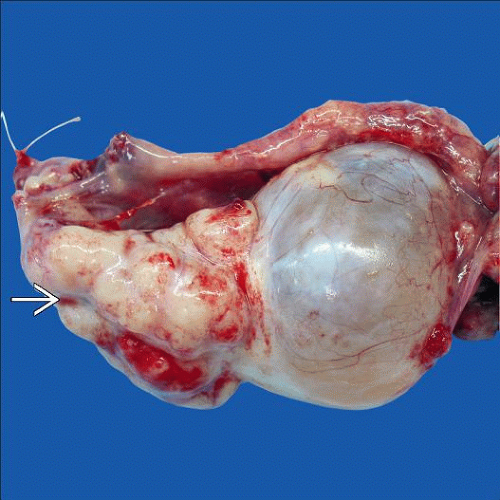
Macroscopic Features
Solid and cystic mass
Tan to white firm cut surface with frequent hemorrhage and necrosis
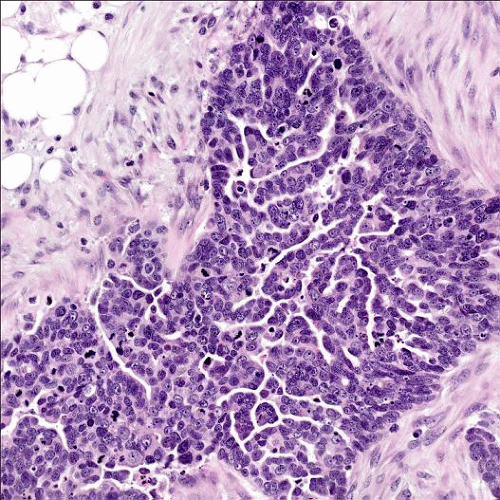
Microscopic Pathology
Hierarchical branching of papillae with cellular tufting and budding
Bridging and fusion of papillae result in slit-like spaces (common)
Solid, pseudoendometrioid, transitional cell carcinoma-like (SET) appearance (BRCA1)
Microcystic and micropapillary patterns (uncommon)
Columnar to cuboidal with eosinophilic, and sometimes clear, cytoplasm
High-grade nuclear atypia, often highly pleomorphic (> 3x variation in size)
Brisk mitoses (typically > 12/10 HPF), often with atypical forms
Ancillary Tests
pax-8, WT1, p16, p53 positive; HNF-1-β negative
Top Differential Diagnoses
Low-grade serous carcinoma
Clear cell carcinoma
Undifferentiated carcinoma
Endometrioid adenocarcinoma
Metastatic endometrial serous carcinoma
TERMINOLOGY
Abbreviations
High-grade serous adenocarcinoma (HGSC)
Synonyms
High-grade serous carcinoma
Definitions
Malignant epithelial tumor showing serous (tubaltype) differentiation, with moderate to severe nuclear atypia
ETIOLOGY/PATHOGENESIS
Familial
BRCA1/BRCA2 germline mutation (18%)
BARD1, BRIP1, CHEK2, MRE11A, PALB2, RAD50, RAD51C, or TP53 germline mutation in 6%
Molecular Alterations
TP53 mutation (> 97%)
Multiple subchromosomal aberrations, most common MYC, CCNE1, NOTCH3 amplification
CLINICAL ISSUES
Epidemiology
Incidence
Most common subtype of surface epithelial ovarian carcinoma
Age
Mean: 6th to 7th decade
Site
Bilateral (60%)
Presentation
Pelvic pain
Increased abdominal girth due to ascites
Gastrointestinal symptoms common
Urinary frequency, dysuria, vaginal bleeding may occur
Asymptomatic (stage I tumors; rare)
Laboratory Tests
Increased serum CA125
Treatment
Bilateral salpingo-oophorectomy + hysterectomy + debulking/staging biopsies
Adjuvant or neoadjuvant chemotherapy
Prognosis
Stage dependent; 30-40% overall 5-year survival
Most patients present with extraovarian disease
Macroscopic disease post surgery most important prognostic factor if advanced stage
Residual tumor < 5 mm in largest focus post neoadjuvant chemotherapy associated with favorable prognosis
MACROSCOPIC FEATURES
General Features
Solid and cystic > solid
Tan to white firm cut surface with frequent hemorrhage and necrosis
Cysts may contain soft, friable papillae and turbid serous to bloody fluid
Surface adhesions and excrescences/nodularity common
Size
Wide range
MICROSCOPIC PATHOLOGY
Histologic Features
Multiple architectural patterns, frequently admixed
Hierarchical branching of papillae with cellular tufting and budding
Bridging and fusion of papillae result in slit-like spaces (common)
Solid
Pseudoendometrioid
Transitional cell carcinoma-like
Microcystic
Glandular
Micropapillary (less common)
Psammoma bodies
Findings after neoadjuvant chemotherapy
Single cells or lobular-like pattern
Clear cell change
Histiocytic reaction and fibrosis
Increased psammoma bodies
Less frequent mitoses
Cytologic Features
Columnar to cuboidal with eosinophilic, and sometimes clear, cytoplasm
High-grade nuclear atypia, often highly pleomorphic (> 3x variation in size)
Signet ring-like cells may be seen
Focal mucinous or squamous differentiation may occur (rare)
Brisk mitoses (typically > 12/10 HPF), often with atypical forms
Tumor infiltrating lymphocytes (more commonly seen with BRCA1 mutation)
ANCILLARY TESTS
Immunohistochemistry
CK7, pax-8, WT1, BER-EP4, MOC-31, B72.3, ER, PR, claudin-4 positive
p53 diffusely positive or completely negative
p16 diffuse strong staining (˜ 60%)
Ki-67 positive usually > 75%
Calretinin may be positive (but only focal)
HNF-1-β negative
DIFFERENTIAL DIAGNOSIS
Low-Grade Serous Carcinoma
Homogeneous bland nuclei with < 3x variation in size
Mitoses ≤ 12 per 10 HPF
Psammoma bodies usually abundant
p53 wild-type pattern, p16 patchy or negative
Clear Cell Carcinoma
Usually low stage
Other typical architectural patterns
Associated endometriosis or adenofibroma
WT1, ER negative; HNF-1-β positive
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree