High-Grade Papillary Urothelial Carcinoma
Jesse K. McKenney, MD
Mahul B. Amin, MD
Key Facts
Terminology
Papillary urothelial neoplasm with moderate to marked nuclear atypia
Clinical Issues
Most occur in 6th decade or later
Strong male predominance (M:F = 6-8:1)
Gross or microscopic hematuria is common
High rate of progression to invasive disease
Microscopic Pathology
Often have complex papillary architecture on low-power examination
Range of nuclear atypia is included in this category
Some have obvious nuclear pleomorphism
Other tumors have more monomorphic nuclei
Some degree of nucleomegaly is present
Irregular clumped nuclear chromatin typical
Neoplastic cells are often crowded and overlapping
Cells lose linear orientation perpendicular to basement membrane
Mitotic activity may be brisk
Cellular discohesion is common
Ancillary Tests
Not required for diagnosis
Top Differential Diagnoses
Low-grade urothelial carcinoma
Papillary-polypoid cystitis
Papillary nephrogenic adenoma
Prostatic-type polyp
Inverted papilloma
Prostatic ductal carcinoma
TERMINOLOGY
Definitions
Papillary urothelial carcinoma with distinct nuclear abnormalities, including presence of moderate to marked nuclear atypia, nucleoli, and pleomorphism
CLINICAL ISSUES
Epidemiology
Age
Most occur in 6th decade or later
Gender
Strong male predominance (M:F = 6-8:1)
Presentation
Gross or microscopic hematuria is common
Urine cytology often shows carcinoma
Treatment
Surgical approaches
Transurethral resection and fulguration of visible tumor
Adjuvant therapy
Intravesical immunotherapy with bacillus Calmette-Guérin (BCG)
Intravesical chemotherapy with thiotepa or mitomycin-C
Prognosis
High rate of progression to invasive disease
MACROSCOPIC FEATURES
General Features
Exophytic papillary growth
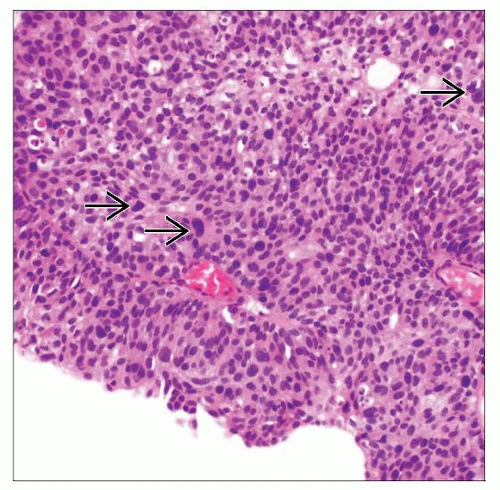
MICROSCOPIC PATHOLOGY
Histologic Features
Often have complex papillary architecture on low-power examination
Anastomosis of papillae and confluence is common
Cellular discohesion and denudation are common
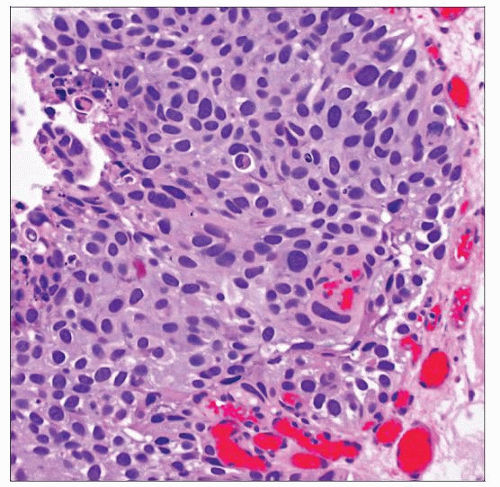
Range of nuclear atypia is included in this category
Some have obvious nuclear pleomorphism
Subset shows marked nuclear anaplasia
Other tumors have more monomorphic nuclei
Nucleomegaly with irregular clumped nuclear chromatin typical
Nuclear rounding is common
Neoplastic cells are often crowded and overlapping
Cells typically lose linear orientation perpendicular to basement membrane (urothelial disorder)
Nuclear contours typically irregular
Mitotic activity may be brisk, including on surface
Nucleoli may be prominent and often in a majority of cells
May be admixed with lower grade foci of carcinoma
ANCILLARY TESTS
Immunohistochemistry
Not required for diagnosis
Expression of CK20 and p53 is more frequent in high-grade carcinomas
Compared to lower grade papillary urothelial neoplasms
DIFFERENTIAL DIAGNOSIS
Low-Grade Urothelial Carcinoma
Nuclear features are less atypical than in high-grade carcinoma
Cells are more uniform in size and evenly distributed at low-power magnification
Nuclei may be rounded
More evenly distributed chromatin
Large nucleoli may occupy some nuclei but are not prominent feature of low-grade carcinoma
Mitoses are variable but not on surface
Cellular discohesion less common
Prominent umbrella cells are occasionally seen
Papillary-Polypoid Cystitis
Broad papillae with stromal edema
Papillae may taper to thin point distally, but base remains broad
Do not have complex secondary or tertiary branching typical of papillary urothelial neoplasia
May have reactive urothelial atypia
Nucleoli and mild nucleomegaly but maintains fine nuclear chromatin
Mitotic activity is common
Clinical impression is usually reactive
Papillary Nephrogenic Adenoma
Papillae are lined by single cuboidal layer
May have other admixed morphologic patterns
Tubular/tubulocystic
May mimic invasion
Diffuse/solid
May mimic poorly differentiated component
Does not have nuclear pleomorphism
Immunoreactivity for pax-2 and pax-8 is characteristic
Prostatic-Type Polyp
Papillae lined by admixed prostatic secretory and urothelial cells
Express PSA and PAP in secretory cell component
Inverted Papilloma
May mimic endophytic growth in high-grade urothelial carcinoma
Thin trabecular architecture without solid expansile growth
Usually maintain prominent basal palisading in nests and trabeculae
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree