Hepatic Neoplasm Ablation and Related Technology
Ido Nachmany
Ravit Geva
DEFINITION
Hepatic ablation represents the use of chemical or physical means to destroy a neoplastic lesion and surrounding normal tissues as an alternative to resection.
INTRODUCTION
The liver is one of the most common sites for development of malignancy—either primary or metastatic disease.
As a general concept, the main curative option for liver tumors is surgical resection via partial hepatectomy or whole liver replacement. A variety of clinical situations preclude this approach; ablation is an attractive and viable option in some of these clinical situations.
The most common indications for liver resection are colorectal cancer liver metastases (CLM), primary liver cancer (mainly HCC and CCA).
In the case of CLM, about 50% of patients will ultimately develop liver metastases. Only about 15% to 20% are resectable at presentation.1
Oncologic benefit of liver resection has been shown only when complete clearance of metastatic disease is achieved.
Factors limiting resection include extent of tumor involvement, volume of the postresection liver remnant, anatomic proximity to essential intrahepatic structures, underlying liver disease, and comorbidities.
HCC is the only universally accepted oncologic indication for liver transplantation (OLT). Only a small subset of patients is suitable for OLT, mainly due to stringent criteria influenced by the limited organ availability and inferior long-term survival in patients with locally advanced disease.
For patients with unresectable liver tumors or those beyond criteria for OLT, life prolongation and control of symptoms are the major goals. This can be achieved by systemic therapy or by different locoregional modalities, grouped under two major categories: tumor ablation and transarterial treatment (chemotherapy infusion, embolization, combination of the two and irradiation).
Ablation can be achieved by direct application of thermal energy (by cooling: cryoablation; heating: radiofrequency ablation [RFA] or microwave ablation [MWA]), chemical ablation: percutaneous acetic acid (PAI) or percutaneous ethanol injection (PEI), or newer techniques: irreversible electroporation (IRE).
The most commonly applied modality is thermal ablation using RFA technique. In recent years, MWA has also been rapidly gaining acceptance.
Based on accumulating data supporting the clinical benefit of ablation techniques, there had been an expansion of the indications. Ablation is now introduced in combination with liver resection and, in limited cases, as a replacement of resection with curative intent.
Ablation can be performed percutaneously, laparoscopically, or via laparotomy.
The main advantage of a percutaneous approach is the minimal invasiveness of the procedure.
The advantages of using ablative modalities in surgery are the ability to reach any territory of the liver, the ability to combine ablation with resection, and the control of inflow and outflow. This may counteract the cooling effect of blood flow in major vessels (referred to as the “heat sink” effect). Laparoscopic ablation may combine the benefits of surgery with those of minimally invasive treatment.
Studying the long-term effectiveness of ablative modalities has been challenging; in part, this is due to the rapid evolution of ablative tools (probes and energy sources), thus the field is in constant development. Also, the results of most studies are limited by sample size, methodology, and followup time.
INDICATIONS
HCC
The vast majority of patients with HCC have background chronic liver disease. The management of these patients takes into account the primary liver disease (synthetic dysfunction and portal hypertension) as well as the extent of the tumor.
The most commonly used algorithm outside of the United States for HCC management is the Barcelona Clinic for Liver Cancer (BCLC) staging and treatment strategy.2 Other criteria (Milan and University of California, San Francisco [UCSF]) have also been forwarded.
Based on the BCLC algorithm, patients suitable for curative treatment are those with very early and early stages (stages 0 and A).
Curative options include resection, liver transplantation, and, in some cases, ablation. The choice between the different options is based on the extent of liver disease, tumor stage, tumor location, and patient comorbidities.
There are three subsets of patients specifically suitable for ablation:
Patients with unresectable HCC beyond transplant criteria. Tumor ablation is usually combined with other treatment modalities, such as transarterial chemoembolization (TACE). These patients are not considered curable.
Patients with very early stage HCC (stage 0—single, up to 2 cm tumor with Child A cirrhosis, and in good performance status) are usually considered resection candidates. Recent data suggest that they can also be managed by ablative modalities. The main potential benefit of resection over ablation is the availability of
the pathologic specimen. The presence of microvascular invasion or microsatellites in the specimen, which are major risk factors for recurrence, is considered by some an indication for “salvage OLT.”3 Therefore, if the patient is a transplant candidate, resection is preferred over ablation. On the other hand, ablation offers a less invasive procedure and may be attractive alternative to patients.
Patients with early stage HCC (stage A—up to 3 lesions, largest ≤3 cm, with Child A-B cirrhosis, and in good performance status) are best treated by OLT unless they have significant comorbidities. In such cases, ablation may be an alternative.
Colorectal liver metastases
The only curative option for patients with CLM is resection, but unfortunately, this is possible in only about 15% to 20% of cases. Some patients may become resectable with neoadjuvant chemotherapy or with anticipated liver remnant volume manipulation such as portal vein embolization.4
The advantages of RFA include low complication rates, fast recovery, and good safety profile in patients with marginal liver reserve. The main disadvantages are the higher local recurrence rates and limitations in treating large or multiple lesions.
Tumor ablation is a valid option for
Patients with limited disease that cannot achieve R0 resection with surgery
Patients who are not surgical candidates due to systemic conditions or because of multiple previous operations on the liver
Some authors consider ablation an alternative in patients with resectable metastases. There are currently no studies to support this approach.5 In the future, with improving devices and technique, the equivalence of ablation and resection may eventually be demonstrated.
Ablation can also be used in combination with resection of other metastases. This is usually done for relatively small and deeply seated lesions for which resection would dramatically increase the morbidity of the procedure.
CONTRAINDICATIONS
There are very few contraindications for ablative therapy.
An absolute contraindication for thermal ablation is abutment of hilar structures, mainly the bile ducts and gallbladder, due to the high risk of thermal injury. This may not apply for IRE.
The vicinity of major blood vessels (specifically hepatic veins and large portal branches) is associated with significantly reduced efficacy due to the heat sink effect and is a risk factor for local recurrence. This can be overcome surgically to some degree by flow manipulation such as the Pringle maneuver or outflow obstruction and thus is not considered an absolute contraindication.
TECHNIQUES
Chemical ablation with injection (usually percutaneously) of ethanol or acetic acid was used mainly for HCC, because this tumor is soft and accepts the fluid injected well. Currently, use of chemical ablation is not common mainly due to inferior efficacy, as compared to thermal ablation and the need for repeated treatments.6
RFA
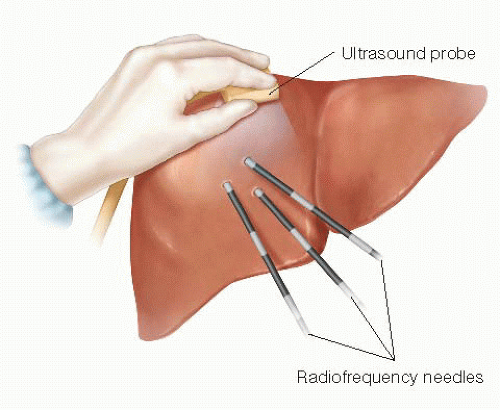
RFA uses alternating electric field delivered through a needle or multiple needle electrodes. It can be inserted percutaneously, laparoscopically, or at laparotomy (FIGS 1 and 2).
Ions in the tissue follow the direction of the rapidly changing current. This causes frictional energy to produce heat and coagulative necrosis.
As temperatures approach 100°C, changes in the physical properties of the tissue increase impedance and limit the flow of current (tissue desiccation due to evaporation of tissue fluid, charring, and the formation of electrically insulating gas between the electrode and the tissue due to boiling). This limits treatment of larger tumors.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree