Overview
In general terms, the topic of hemodynamics deals with flow and distribution of blood and fluids within the body. To maintain the correct amount of intravascular and extravascular volumes, the body must maintain both hydrostatic pressure and osmotic pressure. In vessels, hydrostatic pressure refers to the pressure pushing fluid out into the interstitial tissue. In interstitial tissue, hydrostatic pressure pushes fluid into the vessels. Osmotic pressure, which is imparted by the presence of dissolved solutes, pulls fluid into the vessels and into the interstitial tissue. An imbalance in either of these two pressures results in an abnormal distribution of fluid in the cells or interstitial tissues. The term used to describe excessive amounts of fluid within the interstitial tissues or within cells is edema.
The integrity of vessel walls plays a critical role in maintaining normal distribution of fluid in the vessels and interstitial tissues. The process of coagulation serves to maintain the integrity of the vasculature in the event of disruption of the vascular wall. Inappropriate coagulation can have deleterious consequences, however. For example, abnormal coagulation can result in vessel occlusion; thus the process must be closely controlled. An adequate supply of blood to the tissues is vital because it provides oxygen and nutrients to the cells and removes toxic metabolites from the cells. An inadequate amount of blood flow to an organ is termed ischemia. Ischemia is an important cause of cellular dysfunction and, if severe, often leads to cell death. The resultant area of necrotic cells is termed an infarct. In addition to localized ischemia due to occlusion of blood vessels, a more generalized ischemia can occur due to widespread hypoperfusion of the body. This generalized hypoperfusion of the organs and resultant organ damage is called shock. Shock can result from a decreased amount of blood (i.e., hypovolemic shock), failure of the heart to effectively pump the blood (i.e., cardiogenic shock), or generalized dilation of the vasculature system secondary to infection (i.e., septic shock). This chapter will discuss edema, hyperemia and congestion, hemorrhage, thrombi, emboli, infarcts, and shock.
Edema
Mechanisms of edema formation: Include increased vascular hydrostatic pressure, decreased plasma osmotic pressure, lymphatic obstruction, and inflammation. Increased vascular hydrostatic pressure is usually due to impaired venous return or arteriolar dilation.
- Heart failure: The heart is not pumping blood as effectively as it should, so there is a back up of blood into the veins.
- Cirrhosis: Fibrous scarring of the liver that impairs return of blood through the portal vein, thereby increasing venous pressure in portal vein tributaries and causing fluid to leak into the peritoneal cavity.
- Venous obstruction: For example, a tumor pushing on a vein will cause back up of blood, eventually with leakage of fluid into the interstitium.
- Decreased production of albumin by the liver (e.g., in cirrhosis or other forms of generalized liver damage). A decreased level of albumin results in edema through decreased plasma osmotic pressure. Also, the decreased intravascular volume that accompanies edema stimulates an elevated level of aldosterone. The elevated level of aldosterone, along with several complex changes within the kidney, promotes sodium and water retention. However, because the patient with cirrhosis is hypoalbuminemic, the retained water enters the interstitial space, further contributing to the formation of edema.
- Increased loss of protein by the kidney (e.g., certain glomerular diseases) or in the gut (e.g., protein-losing gastroenteropathy).
- Malnutrition.
Causes of lymphatic obstruction: Lymphoma compressing the thoracic duct or lymphatic channels; certain parasitic infestations, such as elephantiasis.
Inflammation: An important component of acute inflammation is increased vascular permeability, which causes edema.
- In soft tissues of the extremities: Edema usually produces no clinically significant damage. Over time, edema can cause changes in skin, but these are usually only cosmetic.
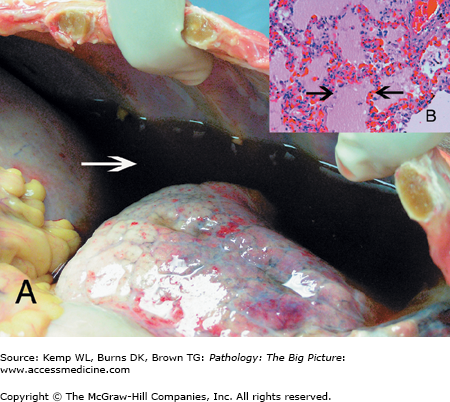
- In the lungs: Edema fluid fills the alveoli and pleural cavities, impairing the ability of the lung to oxygenate the red blood cells (Figure 8-1 A and B).
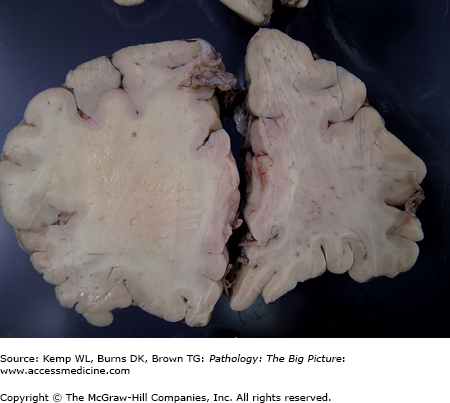
- In the brain: The brain is in a rigid compartment; edema causes the brain to swell, producing increased intracranial pressure (Figure 8-2). When the brain swells, there are only a few places into which it can expand. These expansions of the brain through available spaces are called herniations. Types of herniation include subfalcine, uncal, and cerebellar tonsillar (see Chapter 11 for further discussion of herniation).
Figure 8-1.
Pleural effusion with pulmonary edema. A, Accumulation of fluid in the pleural cavities, or pleural effusions (arrow), may cause respiratory problems by limiting expansion of the lungs. B, Microscopic section from a patient with pulmonary edema. The edema fluid (arrows) stains light pink in this hematoxylin and eosin stained section and fills the alveolar spaces. The presence of fluid within the alveoli interferes with proper oxygenation of blood in the alveolar capillaries. Hematoxylin and eosin, 200×.
Figure 8-2.
Cerebral edema. This patient had a neoplasm on the left side of the brain. The edema of the brain was confined to the left cerebral hemisphere (the site of the tumor), and serves to illustrate the appearance of an edematous versus nonedematous brain. Expansion of the cerebral parenchyma, as seen in the section on the left side of the image, displaces the nonedematous right hemisphere in this case. Various herniation patterns may also occur in this condition. Note the flattening of the crests of the cortical gyri, caused by pressure on the brain from the inner surface of the skull.
- Transudate: Protein and cell-poor fluid that has a specific gravity < 1.012. Cardiac failure or decreased protein levels cause a transudate.
- Exudate: Protein and cell-rich fluid that has a specific gravity > 1.020. Inflammation causes an exudate.
- Dependent edema: Occurs in the extremities and areas of the body where accumulation of fluid is dependent upon gravity. Dependent edema is most commonly associated with heart failure.
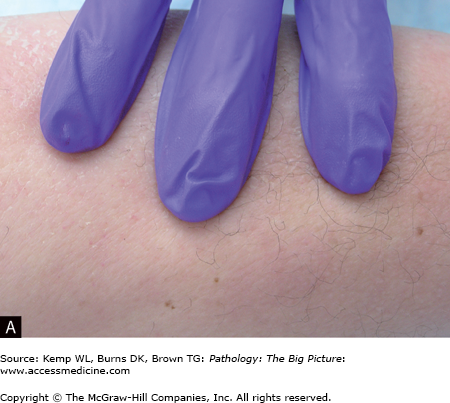
- Pitting edema: When the skin and underlying soft tissues of a leg with edema are compressed with fingers, the impressions remain. This type of edema is most commonly associated with heart failure and is usually a transudate (Figure 8-3 A and B).
- Anasarca: Generalized edema of the entire body that is most commonly associated with glomerular protein loss by the kidneys.
Hyperemia and Congestion
- Hyperemia: Active accumulation of blood within vessels, such as would occur in vasodilation due to acute inflammation.
- Congestion: Passive accumulation of blood within vessels, such as would occur in the lungs due to left-sided heart failure, or in the liver and extremities due to right-sided heart failure.
- Acute passive congestion: Passive congestion that developed recently.
- Chronic passive congestion: Passive congestion that has been occurring over time and is often associated with hemosiderin-laden macrophages and organ damage.
- Hyperemia and acute passive congestion: Blood vessels are dilated by red blood cells; to differentiate the two would require knowledge of the scenario in which it is occurring.
- Chronic passive congestion: A condition due to multiple episodes of acute passive congestion. Red blood cells break down, leaving hemosiderin and stimulate mild inflammation, which results in scarring.
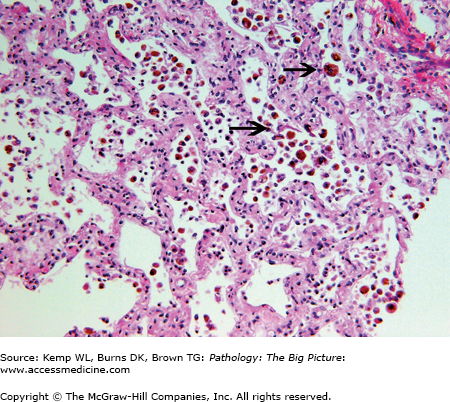
- Cause: Left-sided heart failure, which causes blood to back up into the lungs because the left ventricle is not pumping the blood out as quickly or as efficiently as it should.
- Gross morphology of chronic passive congestion of the lung: Darkly pigmented, heavy and firm lungs.
- Microscopic morphology of chronic passive congestion of the lung: Hemosiderin in macrophages (“heart failure cells”) and fibrosis of the alveolar septae (Figure 8-4).
- Cause: Right-sided heart failure, which causes blood to back up into the liver because the right ventricle is not pumping the blood out as quickly or as efficiently as it should.
- Mechanism of chronic passive congestion of the liver: In this condition, passive congestion of the blood with sinusoidal dilation is associated with a component of hypoxic injury. The sinusoidal dilation and hypoxic injury lead to atrophy and sometimes necrosis of the centrilobular hepatocytes.
- Gross morphology of chronic passive congestion of the liver: Nutmeg liver (shrunken and congested centrilobular areas with raised, tan portal areas) (Figure 8-5).
- Microscopic morphology of chronic passive congestion of the liver: Atrophy of the centrilobular hepatocytes associated with sinusoidal dilation. Fibrosis may be present around the central veins. In cases of severe heart failure or shock caused by other conditions, the centrilobular hepatocytes are frankly necrotic.
Hemorrhage
Petechiae
- Gross morphology: Pinpoint hemorrhages.
- Causes: Include platelet dysfunction and increased vascular pressure (Figure 8-6).
- Gross morphology: Pinpoint hemorrhages.
Purpura
- Gross morphology: Larger than petechiae and usually raised.
- Causes: Commonly associated with vasculitis.
- Gross morphology: Larger than petechiae and usually raised.
Ecchymoses
- Gross morphology: Larger than purpura (> 1.0 cm).
- Causes: Trauma.
- Gross morphology: Larger than purpura (> 1.0 cm).