Hematopoietic and Lymphoid Tissues
Atif Ahmed
▪ Questions and Answers
1. All of the following cell types are found in increased numbers in cases of viral lymphadenitis EXCEPT:
a. Immunoblasts
b. Monocytoid B cells
c. Atypical lymphocytes
d. Reed-Sternberg cells
e. Langerhans cells
View Answer
1. e. In viral lymphadenitis as in the case of infectious mononucleosis, there is follicular and paracortical hyperplasia with proliferation of immunoblasts, tangiblebody macrophages, Reed-Sternberg-like cells, atypical lymphocytes, and monocytoid B cells. Necrosis and viral inclusions can also be seen. Langerhans cells and dendritic cells are not usually prominent. Their presence suggests dermatopathic lymphadenopathy.
2. Associated findings in patients with dermatopathic lymphadenopathy include all of the following EXCEPT:
a. Peripheral blood eosinophilia
b. Hyperplasia of Langerhans and dendritic cells
c. Pruritus
d. Oligoclonal B-cell proliferation
e. Histiocytes laden with melanin pigment
View Answer
2. d. Dermatopathic lymphadenopathy is a proliferation of histiocytes in patchy aggregates in the cortical or the peripheral areas of the lymph node. The paracortical areas are also expanded by Langerhans cells and interdigitating dendritic cells. 70% of patients with dermatopathic lymphadenopathy have cutaneous T-cell lymphoma or Sézary syndrome.
3. Characteristic features of reactive lymphoid hyperplasia include all of the following EXCEPT:
a. Lymphoid follicles of varying sizes
b. Vascular proliferation
c. Hyperplasia of dendritic cells
d. Frequent mitotic figures
e. Overexpression of bcl-2
View Answer
3. e. The size, shape, distribution, and density of the follicles, overexpression of bcl-2, and expression of CD10 in the compressed interfollicular zone in follicular lymphoma help differentiate it from reactive follicular hyperplasia. In reactive hyperplasia, there is proliferation of dendritic cells, histiocytes, tingible-body macrophages, and plasma cells.
4. PML-RARα fusion transcript characteristically results in:
a. Undifferentiated leukemic cells without Auer rods
b. Inv16(p13q22) translocation
c. Chronic leukemia with prominent eosinophils
d. Blast phase of chronic myelogenous leukemia
e. Leukemia with marked coagulopathy
View Answer
4. e. This fusion transcript results in translocation t(5;17)(q22;q11-12), which is a feature of acute promyelocytic leukemia. Leukemic myeloid cells contain characteristic bundles of Auer rods in the cytoplasm, called “faggot cells.” This type of leukemia has good prognosis if treated with transretinoic acid therapy.
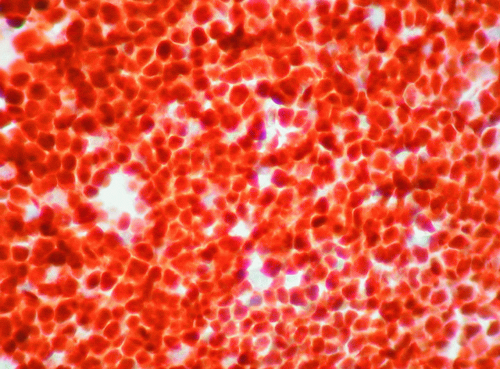
5. What is the immunostain used in this section of a bone marrow from a patient with acute leukemia (Fig. 5.1)?
a. CD3
b. CD20
d. Tdt
e. CD117
View Answer
5. d. Section shows diffuse proliferation of blasts that stain with markers of immature cells such as terminal deoxytransferase (Tdt). Of the list, Tdt is the only nuclear stain and is positive in lymphoblastic leukemia/lymphoma. All the other choices have antibodies that stain the cytoplasm.
6. A most commonly observed feature in patients with Castleman disease is the presence of:
a. CD1a-positive histiocytes
b. Lymphoid hyperplasia with hyalinized germinal centers
c. Lymphoid hyperplasia with numerous plasma cells
d. Immunoglobulin rearrangement of gamma heavy chain
e. Dermatopathic lymphadenopathy
View Answer
6. c. Hyaline-vascular Castleman disease is more common than the plasma cell type, which is seen mainly in multicentric Castleman disease. This disease is sometimes associated with the clonal rearrangements of the T-cell receptor gene, and results in a clinical picture similar to that of angioimmunoblastic lymphadenopathy. It is also associated with herpes virus 8, Kaposi sarcoma, large cell lymphoma, and POEMS (polyneuropathy, organomegaly, endocrinopathy, M-protein, and skin changes) syndrome.
7. Activation of the fusion gene AML1/ETO results in:
a. t(9;11)(p21;q23) translocation
b. Acute lymphoblastic leukemia
c. Leukemic cells with Auer rods
d. Leukemia with biphenotypic profile
e. All of the above
View Answer
7. c. This translocation is one of the most common chromosomal aberrations in acute myeloid leukemia and occurs predominantly in younger patients. Leukemic cells have myeloid differentiation and show cytoplasmic Auer rods. This type of leukemia has good prognosis and good response to chemotherapy.
8. Neoplasms associated with Castleman disease include all of the following EXCEPT:
a. Hodgkin lymphoma
b. Hemangioma
c. Kaposi sarcoma
d. Ewing sarcoma
e. Dendritic follicular tumors
View Answer
8. d. Vascular neoplasms, angiomyoid proliferative lesions, angiomatous hamartomas, and HHV-8 positive Kaposi sarcoma have all been reported to occur in patients with Castleman disease. Ewing sarcoma is not associated with Castleman syndrome.
9. Which population has the highest frequency of Rosai-Dorfman disease (sinus histiocytosis with massive lymphadenopathy)?
a. White women
b. White men
c. Elderly African Americans
d. Young African Americans
e. Hispanic Americans
View Answer
9. d. Rosai-Dorfman disease is mainly seen in young African American children and adolescents. It presents as neck lymphadenopathy and also involves the extranodal areas in one fourth of cases. It is a benign histiocytosis characterized histologically by engulfment of lymphocytes. Phagocytic cells are reactive with S-100 but not with CD1a or Epstein-Barr viral markers.
10. What is the most common lymphoma seen in children?
a. Lymphoblastic lymphoma
b. Classical Hodgkin lymphoma
c. Nodular lymphocyte predominant Hodgkin lymphoma
d. Diffuse large B-cell lymphoma
e. Burkitt lymphoma
View Answer
10. a. Lymphoblastic lymphoma is the most common lymphoma type in children and is usually of the T-cell type. It presents with mediastinal mass with or without lymphadenopathy. It is a high-grade lymphoma that is typically positive for Tdt and not CD30.
11. Of the following histologic types of Hodgkin lymphoma, which one has the WORST prognosis?
a. Nodular sclerosis classical Hodgkin lymphoma
b. Mixed cellularity
c. Lymphocyte-depleted type
d. Lymphocyte-rich
e. Lymphocyte-predominant type
View Answer
11. c. The prognosis of Hodgkin lymphoma is best in nodular sclerosis type, followed by mixed cellularity. The overall 5-year survival rate for Hodgkin lymphoma is 75%, and is worst in lymphocyte-depleted type.
12. The most important prognostic parameter in Hodgkin disease is:
a. Age
b. Race and gender
c. Clinical stage
d. Location
e. Histologic type
View Answer
12. c. Clinical stage is the most important prognostic parameter. Stage IV has the worst prognosis. African Americans men, mediastinal tumor, splenic nodules, lymphocyte depletion, and age more than 50 years are other parameters associated with poor prognosis. Favorable prognostic features in Hodgkin lymphoma include female gender, white race, nodular lymphocyte-predominant, and nodular sclerosis histologic types.
13. Classic CD 30+, CD15+ Reed-Sternberg cells are found in all of the following subtypes of Hodgkin disease EXCEPT:
a. Fibrotic nodular sclerosis
b. Interfollicular variant
c. Fibroblastic
d. Eosinophilic microabscesses
e. Nodular lymphocyte predominance
View Answer
13. e. Unlike other types of Hodgkin, nodular lymphocyte-predominant Hodgkin lymphoma cells are negative for CD30 and CD15 and stain with CD20, CD79a, and BSAP.
14. Which of the following statements are correct regarding refractory anemia with ringed sideroblasts (RARS)?
a. It is commonly caused by parvovirus infection.
b. Bone marrow is hypocellular and shows depletion of the erythroid series.
c. Abundant hemosiderin-laden macrophages are present in the bone marrow.
d. Evolves to acute leukemia in 50% of cases.
e. It characteristically occurs in children.
View Answer
14. c. Refractory anemia with ringed sideroblasts (RARS) characteristically affects older individuals and shows evidence of iron overload in the bone marrow, spleen, and liver. It is an idiopathic disease that can only be diagnosed after excluding all other possible etiologies of erythroid abnormalities. It evolves to acute leukemia in 1% to 2% of cases.
15. BCR/ABL gene fusion at the major breakpoint cluster region leads to all of the following events EXCEPT:
a. Clonal hematopoietic cell proliferation
b. Downregulation of tyrosine kinase activity
c. Enhanced transcription of MYC and BCL-2 genes
d. The formation of a p210 protein
e. Chronic leukemia
View Answer
15. b. In chronic myelogenous leukemia, the breakpoint in the BCR gene is in the major breakpoint cluster region (BCR exons 12-16) and a p210 protein is formed. The fusion gene leads to increased tyrosine kinase receptor activity. Inhibition of tyrosine kinase by Gleevec is a mode of treatment of chronic myelogenous leukemia.
16. Evolution of chronic myelogenous leukemia to a phase of worse prognosis is heralded by all of the following events EXCEPT:
a. Presence of bone marrow blasts of lymphoid origin, >20% of cells
b. Gain of additional chromosomal abnormalities
c. Drop in absolute neutrophil count
d. The appearance of pseudo-Gaucher cells
e. Increase in the size of the spleen
View Answer
16. c. Blast phase of chronic myelogenous leukemia resembles acute leukemia where the number of blasts exceeds 20%. The blast lineage is mostly myeloid but can be lymphoblastic in 20% of cases. There is gain of additional chromosomal abnormalities. Splenomegaly, thrombocytosis, and thrombocytopenia are seen in both accelerated and blast phases. The white cell count does not decrease.
17. Isolated deletion of chromosomal region 5q (5q- syndrome) typically leads to:
a. Acute leukemia in children
b. Essential thrombocythemia
c. Worsening prognosis in chronic lymphocytic leukemia
d. Myelodysplastic syndrome in elderly white men
e. Refractory anemia
View Answer
17. e. Monosomy 5q- syndrome characteristically occurs in women and causes myelodysplastic syndrome with blasts <5%. The disease leads to refractory anemia and increase in megakaryocytes with hypolobated nuclei. Isolated monosomy 5 syndrome is associated with good survival.
18. Progressive transformation of germinal centers is associated with which of the following conditions?
a. Measles
b. Toxoplasmosis
c. Syphilitic lymphadenitis
d. Nodular lymphocyte-predominant Hodgkin disease
e. Castleman disease
View Answer
18. d. Progressive transformation of germinal centers describes an alteration of lymphoid architecture in which lymphoid follicles become enlarged and infiltrated by small lymphocytes. It occurs in association with nodular lymphocyte-predominant Hodgkin disease and other reactive lymphadenopathies.